Topical vs. Oral Meds: Which Is Safer and How Much Gets Into Your Bloodstream?
 Jan, 24 2026
Jan, 24 2026
When you reach for a pain reliever, do you think about how it gets into your body? Most people don’t-until they get sick from it. That’s where the real difference between topical meds and oral pills becomes life-changing.
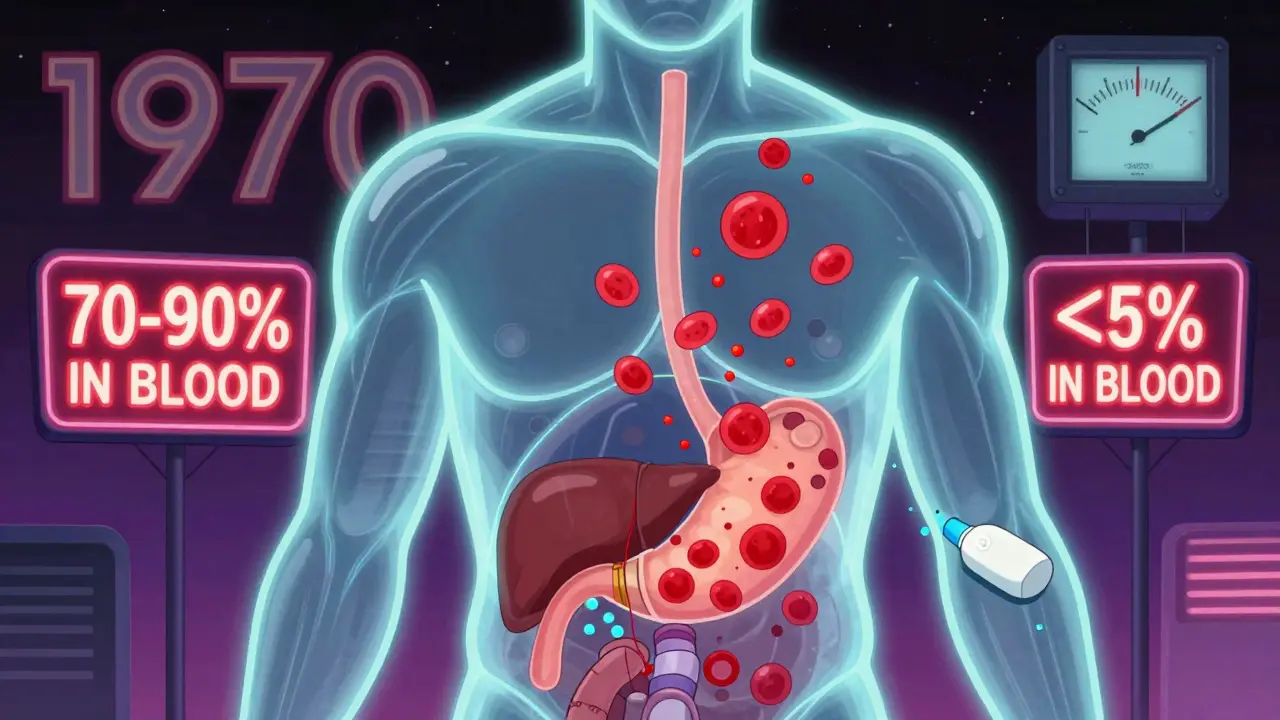
Take NSAIDs, the most common painkillers. If you swallow ibuprofen or naproxen, your stomach and liver get the first hit. About 70-90% of the drug enters your bloodstream. That’s great if you need full-body relief. But it’s dangerous if you’re over 65, have a history of ulcers, or take other meds. The FDA says 18,432 people were hospitalized in 2023 just from oral NSAID stomach bleeding. That’s not a rare side effect. It’s predictable.
Now compare that to a topical gel. You rub diclofenac on your knee. Less than 5% of that dose ever reaches your blood. The rest stays right where you put it-right in the sore joint. That’s not magic. It’s physics. Your skin is a barrier. And modern gels are designed to respect that barrier, not break through it.
How Much Actually Gets Into Your Blood?
It’s not a yes-or-no question. It’s a matter of degrees.
Oral meds go straight into your digestive tract. From there, they’re absorbed into the portal vein and sent to your liver. That’s called first-pass metabolism. Your liver breaks down a chunk of the drug before it ever reaches the rest of your body. For some drugs, like morphine, up to 95% gets destroyed. For others, like acetaminophen, it’s only 15%. On average, you lose nearly 60% of the dose before it even starts working.
Topical meds? They don’t go through your gut or liver at all. At least, not at first. Most of it stays in the skin. But here’s the catch: some still gets in. How much? It depends.
A standard cream or gel delivers less than 5% of the dose into your blood. That’s why the risk of stomach ulcers drops from 15% with pills to under 1%. But if you apply it to a huge area-say, your whole back-or if your skin is cracked or thin, that number can jump. One study found patients using large amounts of topical diclofenac had blood levels high enough to cause liver stress. It’s rare, but it happens.
Transdermal patches are different. They’re designed to get through the skin. Fentanyl patches? They deliver 92% of the drug into your blood over three days. That’s not topical. That’s systemic delivery in disguise. Don’t confuse the two.
Why Topical Is Safer-And When It’s Not
The safety advantage isn’t theoretical. It’s in the numbers.
The American College of Rheumatology says topical NSAIDs should be the first choice for knee or hand osteoarthritis. Why? Because they work just as well for localized pain, but cause 78% fewer serious side effects. In a 2023 survey of over 2,400 arthritis patients, 89.7% preferred the gel because they didn’t get stomach pain. Only 42.3% of oral users said the same.
But here’s what no one tells you: topical doesn’t mean zero risk. About 10-15% of users get a rash or itching where they apply it. That’s contact dermatitis. It’s annoying, but it’s not life-threatening. The real danger? Thinking you’re completely safe.
If you’re using a topical NSAID on your shoulder, your hip, and your lower back-all at once-you’re not using a local treatment anymore. You’re giving yourself a full-body dose. That’s how people end up with kidney damage or high blood pressure from topical meds. The skin isn’t a perfect wall. It’s a sieve. And if you pour too much through it, it leaks.
What Oral Meds Do Better
Topical isn’t always the answer. If your pain is inside your body-like a kidney stone, a stomach ulcer, or a systemic infection-you need the drug in your blood. That’s where oral meds win.
Antibiotics? You can’t rub them on a lung infection. Topical antibiotics work great for a cut or acne, but for pneumonia? You need the pill. Same with thyroid meds, blood pressure drugs, or antidepressants. They have to reach organs your skin can’t touch.
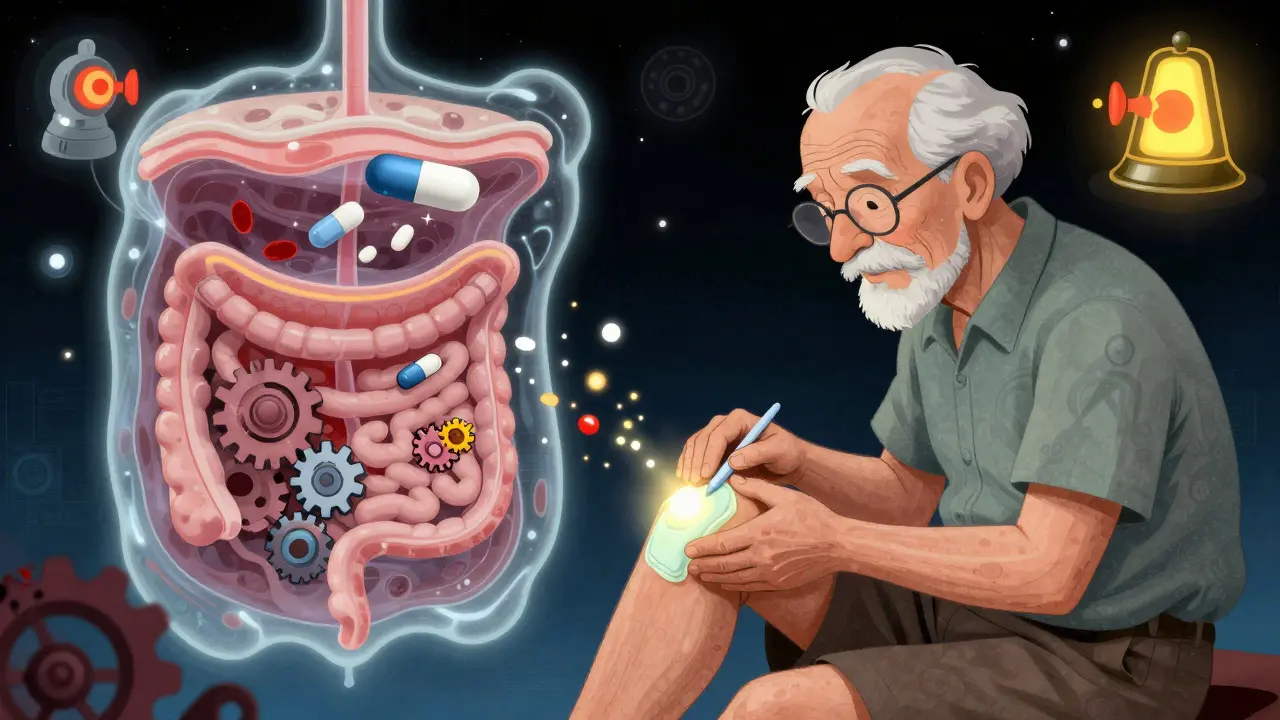
And let’s be honest: swallowing a pill is easier than applying gel three times a day. If you’re elderly, have arthritis in your hands, or just hate the mess, oral is more convenient. That’s why adherence rates for oral meds are higher in some groups-unless you’re dealing with side effects. Then, people drop them fast.
One study found 78% of people quit oral NSAIDs within six months because of stomach issues. Only 22% stopped the gel. And of those who did? Most said it just didn’t work well enough for their pain.
Real-World Problems You Won’t Find in Brochures
Here’s what patients actually struggle with:
- “It takes too long to work.” Topical gels can take 30-60 minutes to start helping. Pills kick in in 20. If you’re in acute pain, that delay matters.
- “It’s messy.” You get grease on your clothes. Your hands smell like medicine. You have to wait before touching anything. Reddit users in r/ChronicPain posted 214 complaints about this in just one month.
- “It doesn’t work in the cold.” Skin absorption slows when it’s cold. If you live in Minnesota and your knee hurts in winter, the gel might not penetrate as well. Warming the area helps-but most instructions don’t say that.
- “I didn’t use enough.” A 2023 pharmacist survey found 41% of topical treatment failures were because people used too little. You need a 4-6 inch ribbon of gel, not a dime-sized blob. Most people don’t know that.
Oral meds have their own headaches. Food can block absorption. Levothyroxine? Take it with breakfast and you might get half the dose. Grapefruit juice? It can turn a safe dose into a toxic one. And if you forget a pill? You’re off schedule. Topical gels are more forgiving-if you miss a dose, you just apply it next time.
Who Should Use What?
There’s no one-size-fits-all. But here’s a simple guide:
- Use topical if: Your pain is in one joint (knee, elbow, wrist), you’re over 65, you have a history of stomach ulcers, or you’re on blood thinners.
- Stick with oral if: You have widespread pain (like fibromyalgia), internal inflammation (like rheumatoid arthritis), or an infection that needs systemic treatment.
- Ask your doctor about patches if: You need steady, long-term pain control (like back pain or neuropathy) and can’t tolerate pills.
- Avoid topical if: You have open wounds, severe eczema, or are applying it to more than 10% of your body surface area.
The American Geriatrics Society says this clearly: for seniors, topical NSAIDs are safer than oral ones. Period. And Medicare now covers 82% of topical NSAID prescriptions-more than oral. That’s not random. It’s because hospitals are seeing fewer bleeding cases.
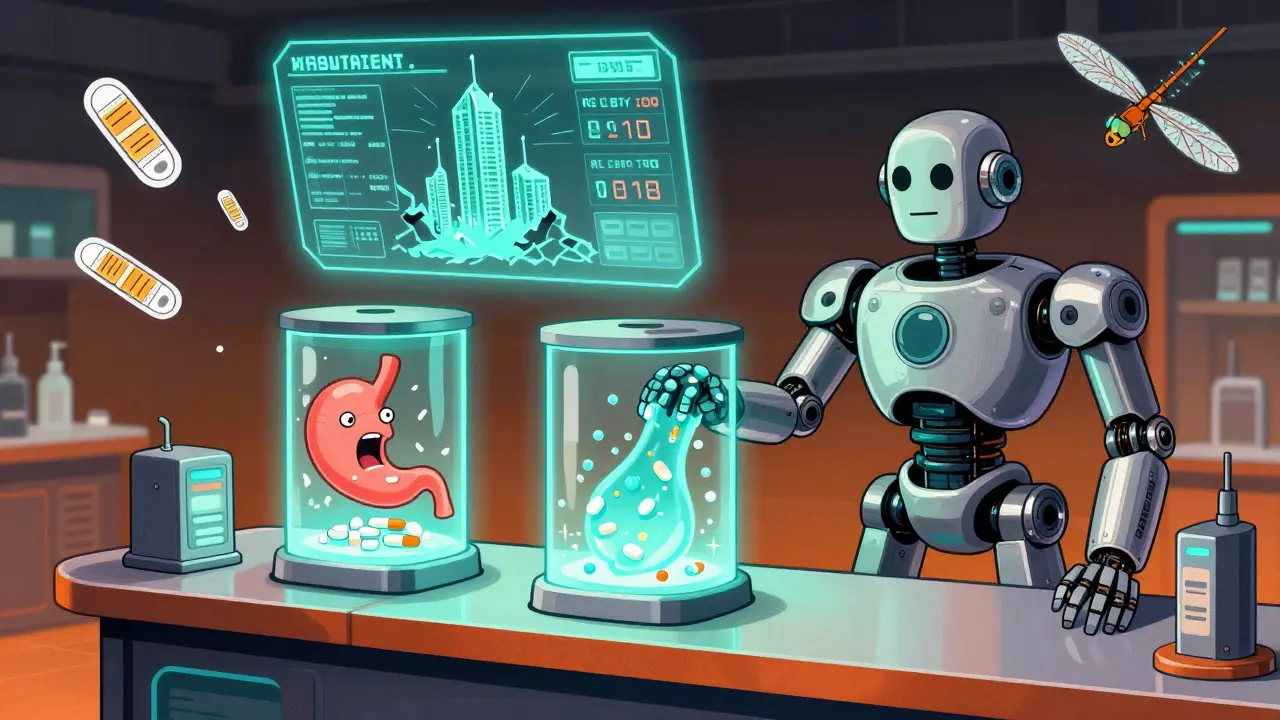
The Future: Patches, Microneedles, and Smarter Gels
The next five years will change everything.
Companies are now making gels that use tiny chemical boosters to push more drug through the skin-without increasing blood levels dangerously. The FDA approved a new diclofenac gel in 2023 that penetrates 3 times deeper than older versions-but still keeps blood levels under 5% of the oral dose.
And then there are microneedle patches. These are tiny needles, smaller than a human hair, that poke through the top layer of skin and release medicine slowly. In trials, they’ve delivered osteoporosis drugs-medicines that used to only work as pills-with 45% bioavailability. That’s huge. It means we might soon have patches for drugs that were once thought impossible to deliver topically.
But here’s the catch: the skin still blocks large molecules. Anything over 500 Daltons (a unit of molecular weight) struggles to get through. That’s why insulin, biologics, and most antibiotics still need injections or pills. The barrier isn’t broken. It’s just being smarter about how we work with it.
Final Takeaway: Choose Based on Risk, Not Convenience
Topical meds aren’t a miracle. But they’re a major step forward in medication safety. If you’ve ever had stomach pain from an NSAID, you know why.
The goal isn’t to avoid all drugs. It’s to get the benefit with the least harm. For localized pain, topical delivers that. For full-body conditions, oral still wins.
Don’t assume topical is always safe. Don’t assume oral is always necessary. Talk to your pharmacist. Ask: “Is this drug meant to stay local-or does it need to get into my blood?” That one question can save you from a hospital stay.
The data doesn’t lie. Fewer side effects. Fewer hospital visits. More people sticking with their treatment. That’s the real win.
Can topical medications cause side effects like oral ones?
Yes, but much less often. Topical NSAIDs rarely cause stomach bleeding or kidney damage because they don’t flood your bloodstream. But they can cause skin rashes, itching, or burning at the application site. In rare cases-like applying large amounts over broken skin or using them daily for months-they can still cause systemic side effects, including high blood pressure or liver stress. Always follow the dosage instructions.
Are topical pain relievers as effective as pills?
For localized pain-like a sore knee, elbow, or wrist-yes. Clinical studies show topical NSAIDs work just as well as oral ones for these conditions. But for widespread pain (like arthritis in multiple joints) or internal pain (like a stomach ache or headache), pills are more reliable. Topical meds don’t reach deep tissues or organs effectively.
Why do some topical gels work better than others?
It’s all about the formulation. Gels with penetration enhancers (like Diclonate P) deliver more drug into the skin and deeper tissues. Liposomal gels and creams with specific carriers (like dimethyl sulfoxide or ethanol) also improve absorption. Basic over-the-counter creams without these enhancers often deliver less than 2% of the dose into the tissue. Always check the active ingredient and whether it’s a newer, enhanced formula.
Can I use topical and oral NSAIDs together?
Not without talking to your doctor. Combining them increases your total NSAID exposure, even if the topical dose seems small. You could end up with the same risks as taking pills alone-stomach ulcers, kidney strain, or heart problems. If you’re using both, your doctor should monitor you closely.
Is it safe to use topical meds long-term?
For most people, yes-but with limits. Long-term use (over 3 months) should be reviewed by a doctor. While the risk of internal damage is low, skin irritation can build up, and repeated use on large areas may lead to unnoticed systemic absorption. The FDA recommends using topical NSAIDs only for short-term relief unless otherwise directed. If you need daily pain relief for more than 30 days, consider alternatives.
What should I do if my topical gel doesn’t work?
First, make sure you’re using enough. Most people under-dose. Use a 4-6 inch ribbon, apply it 3-4 times daily, and rub it in gently. Wait 30 minutes to feel relief. If it still doesn’t help, your pain may be too deep or widespread for topical treatment. Talk to your doctor-you might need an oral option, physical therapy, or another approach. Don’t just keep applying more gel.
rasna saha
January 25, 2026 AT 22:08I’ve been using diclofenac gel for my knee for six months now, and honestly? No more stomach nightmares. I used to dread taking pills after lunch-felt like my insides were being sandblasted. This? Just rub it on, smell like a pharmacy for five minutes, and move on. Life’s too short for GI drama.
Kipper Pickens
January 27, 2026 AT 15:42Let’s not conflate transdermal with topical. The FDA classifies patches as systemic delivery devices-fentanyl, nitroglycerin, estrogen-they all bypass first-pass metabolism and achieve near-complete bioavailability. Topical gels? That’s local pharmacokinetics with minimal systemic exposure. Confusing the two is like calling a bicycle a motorcycle because both have wheels. The mechanism matters.
Also, penetration enhancers like DMSO or ethanol in newer formulations aren’t ‘magic’-they’re surfactants that disrupt stratum corneum lipid packing. That’s why enhanced gels hit 4-5% bioavailability versus 1-2% in OTC creams. It’s not marketing. It’s biopharmaceutics.
Skye Kooyman
January 29, 2026 AT 13:14shivam utkresth
January 30, 2026 AT 21:04Man, I love how this post breaks it down without the usual medical BS. In India, most folks just swallow pills like candy-no idea what’s happening inside. I showed my dad this and he finally stopped taking ibuprofen every day after his ulcer scare. He switched to the gel for his shoulder and now he’s actually talking about going for walks again. Small wins, right?
Also, the ‘cold weather doesn’t work’ thing? 100% true. My aunt in Delhi uses the gel year-round but swears it’s useless in winter unless she warms it in her palms first. No one tells you that. Pharma companies sure don’t print it on the tube.
Aurelie L.
January 31, 2026 AT 15:54TOPICAL IS A SCAM. I used it for my back pain for three weeks. Zero effect. Then I took one pill and felt like a new person. All that rubbing? Just a fancy way to waste time and money. If it doesn’t work, it doesn’t work. Stop pretending it’s ‘safer’ when it’s just weaker.
Joanna Domżalska
February 2, 2026 AT 11:27So we’re supposed to believe that applying something to skin is ‘safer’ but then you admit that if you use too much, it’s just as bad? That’s not science. That’s a marketing loophole. If the drug gets into your blood, it’s systemic. If it’s systemic, it’s not ‘topical.’ You’re just rebranding pills as lotion to sell more. Wake up.
Faisal Mohamed
February 2, 2026 AT 12:53Micro needles = future 💪🧠
Imagine a patch that delivers insulin without needles. Or antibiotics for pneumonia without swallowing a pill. The skin isn’t a wall-it’s a gateway. We’re just learning how to knock. 🤖💊
James Nicoll
February 3, 2026 AT 00:34Oh wow, so the ‘safe’ option is the one that takes 45 minutes to work, leaves grease on your shirt, and you have to remember to rub it on three times a day? Meanwhile, the ‘dangerous’ option is just pop a pill, forget about it, and go about your life?
Let me guess-this article was sponsored by the topical gel company. Because nothing says ‘patient-centered care’ like making elderly people with arthritis rub cream on their hips for 10 minutes every morning. I’m sure they’re thrilled.
Uche Okoro
February 3, 2026 AT 08:18Empirical data confirms that topical NSAID bioavailability is inversely proportional to stratum corneum integrity and directly proportional to application surface area. The 5% threshold is a population mean, not an absolute ceiling. When applied to compromised skin (e.g., eczematous, aged, or irradiated dermis), transcutaneous flux can exceed 12%-sufficient to inhibit hepatic CYP2C9 and elevate serum creatinine. This is not anecdotal. It is pharmacokinetic fact.
Furthermore, concurrent use of occlusive dressings increases absorption by 2.8-fold (per J Clin Pharmacol 2022). Therefore, the assertion that topical = safe is statistically and physiologically untenable without context. Misapplication is systemic exposure in disguise.
Ashley Porter
February 4, 2026 AT 15:08Just want to add: the new diclofenac gel with Diclonate P? Game changer. I used the old stuff for years and it barely touched my knee pain. Switched to the enhanced formula-felt it in 20 minutes. No stomach issues. No mess. Just pure relief. If you’ve written off topical because of bad experiences, try the newer ones. They’re not the same product.
Peter Sharplin
February 5, 2026 AT 20:49Biggest mistake people make? They think topical = no risk. Nope. It’s just a different risk profile. Skin irritation? Annoying. But systemic absorption from overuse? That’s the silent killer. I’ve seen two patients in my clinic with acute kidney injury from applying topical NSAIDs to their entire back for six months. No one told them it was cumulative.
Also, the 4-6 inch rule? Crucial. Most people use a pea-sized blob. That’s 1/10th the dose. You’re not getting relief-you’re wasting money. If you’re not seeing results, check your application technique before giving up. And if you’re using it on more than one joint? Talk to your pharmacist. Dose stacking is real.
Kipper Pickens
February 6, 2026 AT 20:04James Nicoll’s sarcasm is spot-on, but the real issue isn’t convenience-it’s adherence. People quit pills because they’re toxic. They quit gels because they’re inconvenient. The solution isn’t to vilify topical-it’s to improve delivery. Microneedles, transdermal patches with timed release, even wearable patches that vibrate to remind you to reapply? That’s the future. Not ‘take a pill’ vs ‘rub cream.’ It’s ‘get the drug where it needs to go, with zero side effects.’