Stability Testing: How Pharmaceutical Companies Monitor Drug Quality Long After Manufacturing
 Dec, 24 2025
Dec, 24 2025
When you pick up a bottle of pills from the pharmacy, you assume they’ll work exactly as intended - even if they’ve been sitting on the shelf for a year. But how do manufacturers know that? It’s not luck. It’s stability testing.
Stability testing isn’t just paperwork or a regulatory checkbox. It’s the backbone of drug safety after production ends. Imagine a heart medication losing potency over time, or an antibiotic breaking down into something toxic. That’s not theoretical - it’s happened. In 2021, nearly 1 in 6 drug recalls in the U.S. were tied to stability failures. Stability testing exists to stop that before it reaches you.
What Exactly Is Stability Testing?
Stability testing is the process of tracking how a drug changes over time under real-world conditions. It answers one simple question: Will this medicine still be safe and effective when you take it six months, two years, or even five years from now?
The testing isn’t done in a lab for a few days. It’s done in controlled chambers that mimic the environment where the drug will be stored - whether that’s a pharmacy shelf, a home medicine cabinet, or a warehouse in a humid climate. These chambers hold temperature and humidity at precise levels: 25°C and 60% relative humidity for most markets, or 30°C and 65% for hotter regions. Samples are pulled at regular intervals - 0, 3, 6, 12, 24, and 36 months - and tested for changes.
What do they test? Everything. The color, texture, and smell. The pH level. The amount of active ingredient left. The presence of breakdown products. Even how quickly the pill dissolves in the body. All of it. And every test method must be validated to catch even tiny changes. A single tablet can go through dozens of tests over its lifetime.
Why This Isn’t Optional - It’s the Law
Stability testing isn’t something companies do because they’re nice. It’s required by law. The International Council for Harmonisation (ICH), formed in 1990 by regulators from the U.S., Europe, and Japan, set the global standard with ICH Q1A(R2). This guideline says: no shelf life, no approval.
Every New Drug Application (NDA) and Abbreviated New Drug Application (ANDA) submitted to the FDA must include full stability data. Without it, your drug doesn’t get approved. The data isn’t just for the regulator - it’s for the label. The expiration date printed on your bottle? That’s not a guess. It’s based on real data showing when the drug drops below 90% potency or exceeds safe limits for impurities.
And it’s not just about the U.S. The European Medicines Agency, Health Canada, and Japan’s PMDA all follow the same ICH rules. If you want to sell your drug globally, you follow these standards - or you don’t sell at all.
How Much Does It Cost - And Why?
Stability testing is expensive. A single product study can cost between $50,000 and $150,000. For a company with 20 products, that’s over $1 million a year just on testing. Add in the chambers, sensors, calibration, staff, and data systems, and annual investment often hits $2 million.
Why so much? Because it’s slow. Real-time testing takes years. You can’t speed it up without risking accuracy. Accelerated testing at 40°C and 75% humidity gives you a hint - but it’s not a guarantee. A 2021 study in the Journal of Pharmaceutical Sciences found that accelerated data often overestimates shelf life by months, sometimes years.
And it’s not just about time. Each chamber must be qualified every three months. Temperature mapping studies cost about $8,500 per unit. Calibration needs to be ISO 17025 accredited. One humidity spike in a chamber can wipe out six months of data - and delay an entire product launch by months. One company lost $2.3 million because of a single chamber failure.
Who Does It - And How?
Big pharma companies like Pfizer, Merck, and Novartis run their own stability labs. They have entire departments dedicated to it. But smaller companies? They outsource. About 72% of pharmaceutical firms now use Contract Research Organizations (CROs) like SGS, Eurofins, or Charles River Laboratories.
These CROs specialize in stability testing. They have the chambers, the staff, the validated methods, and the audit trails. For a small biotech, paying $150,000 to $500,000 a year for outsourced testing is cheaper than building and maintaining their own facility.
Inside the lab, it’s not just technicians running tests. It’s chemists using HPLC and GC-MS to detect trace impurities. Statisticians using JMP or Minitab to calculate shelf life with 95% confidence. Regulatory specialists making sure every document meets ICH Q1A(R2) requirements - which include at least 15 elements in the protocol and 20 in the final report.
The Hidden Value: Preventing Recalls and Saving Lives
Most people think stability testing is about compliance. It’s not. It’s about prevention.
The International Pharmaceutical Aerosol Consortium found that between 2020 and 2022, stability testing blocked 47 unsafe drugs from reaching the market. Why? Because they found unexpected degradation products - chemicals formed as the drug broke down. Some were toxic. Others made the medicine ineffective.
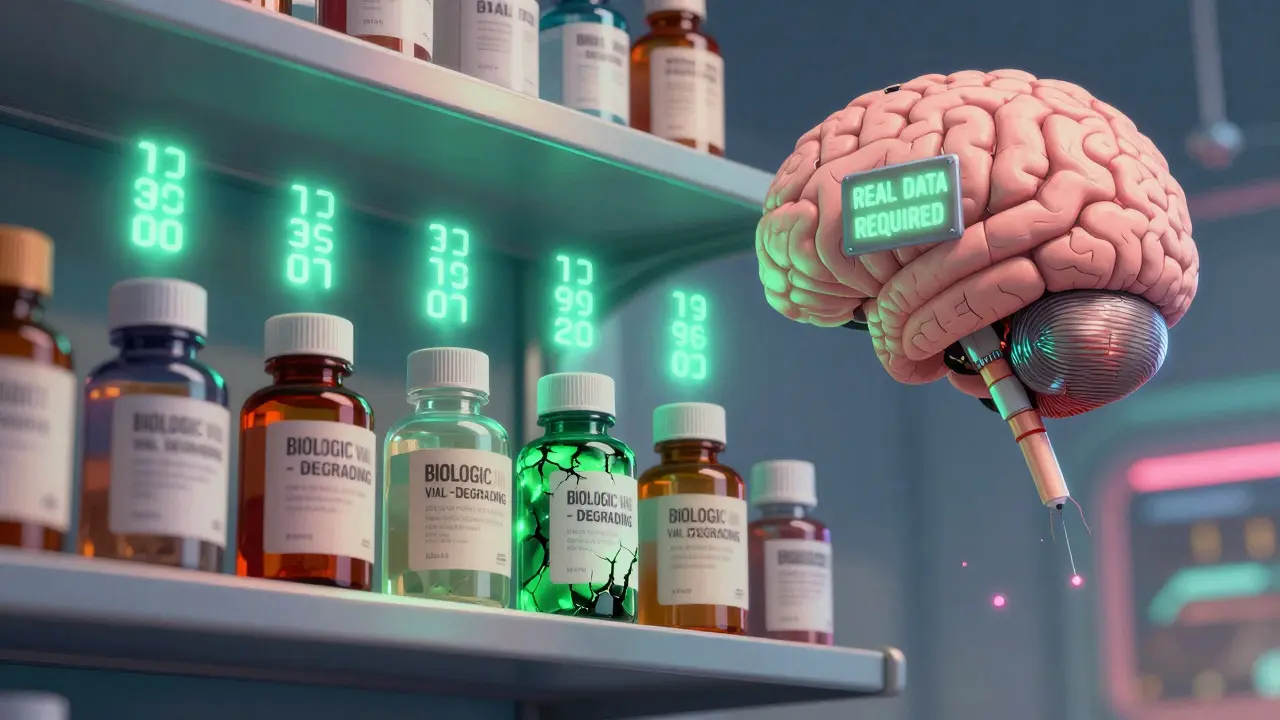
One case from SGS in 2022 saved a $500 million product. A new biologic drug looked fine in early tests - until stability testing revealed it was reacting with its glass vial. The drug was absorbing into the container. That’s not something you catch in a 3-day pilot test. Only long-term monitoring found it. The company redesigned the packaging before launch.
Dr. Jennifer Orme of Pfizer said robust stability programs cut post-market recalls by 31% since 2015. That’s not just money saved. That’s patients protected.
Challenges and Controversies
Not everyone thinks the system is perfect. Dr. Robert Elder, a consultant for generic drug makers, argues that for simple, stable small-molecule drugs - like aspirin or metformin - the 36-month real-time test is overkill. He says it adds 18 to 24 months to development with little added safety benefit.
He’s not wrong. For well-understood drugs, there’s growing support for risk-based testing. ICH Q12, introduced in 2018, allows companies to use data from earlier stages and change testing protocols after approval - without re-submitting to regulators. About 43% of major pharma companies now use these principles to reduce sample sizes by up to 40%.
Still, regulators are cautious. A 2021 FDA warning letter cited a company that ignored out-of-spec results on a cancer drug. They delayed testing and failed to investigate. Approval was delayed by 14 months. That’s the risk of cutting corners.
The Future: Faster, Smarter, More Predictive
The field is changing. In February 2023, ICH finalized Q13, a new guideline for stability testing in continuous manufacturing - a shift away from batch-based production. By 2025, companies will need to monitor stability in real time during production, not just after.
Artificial intelligence is coming fast. Machine learning models can now predict degradation pathways based on chemical structure, environmental data, and historical results. PhRMA predicts AI will cut testing timelines by 30-40% by 2027. Imagine running a virtual 36-month test in 3 weeks.
But here’s the catch: regulators won’t let AI replace real data - not yet. It can guide testing, reduce sample numbers, and flag risks - but the final expiration date still needs real-world proof.
And as drugs get more complex - biologics, gene therapies, personalized medicines - stability testing becomes even more critical. These drugs degrade faster, react unpredictably, and are harder to analyze. The demand for advanced testing is growing faster than ever.
What You Should Know
If you’re a patient: Trust that your medicine has been tested. The expiration date isn’t arbitrary. It’s the result of years of science and millions of dollars in testing.
If you’re in the industry: Don’t treat stability testing as a cost center. It’s a risk management tool. A single failure can cost more than a decade of testing.
If you’re a student or new professional: Learn the ICH guidelines. Master HPLC. Understand statistical analysis. Stability testing isn’t glamorous - but it’s where the real work of patient safety happens.
Stability testing doesn’t make headlines. But every time a drug works as it should - even after sitting on a shelf for years - that’s its quiet victory.
How long does stability testing usually take for a new drug?
For a new drug, full real-time stability testing typically takes 24 to 36 months to complete. Samples are tested at intervals like 0, 3, 6, 12, 18, 24, and 36 months. Accelerated testing at 40°C and 75% humidity runs for 6 months and helps predict long-term behavior, but it doesn’t replace real-time data for setting expiration dates.
What happens if a drug fails stability testing?
If a drug fails - meaning it falls outside pre-set quality limits for potency, purity, or physical properties - the manufacturer must investigate the cause. This triggers an out-of-specification (OOS) investigation under cGMP rules. Depending on the cause, the product batch may be rejected, the shelf life shortened, the packaging changed, or the formulation reformulated. In severe cases, regulatory agencies may delay approval or issue a recall if the drug is already on the market.
Are stability requirements the same for all types of drugs?
No. Traditional small-molecule drugs like pills and capsules follow standard ICH Q1A(R2) conditions. But biologics - like vaccines, antibodies, or gene therapies - are far more sensitive. They often require colder storage (2-8°C), more frequent testing, and specialized analytical methods. Some biologics degrade within weeks, so their stability protocols are much more intensive and customized. ICH guidelines have separate annexes for these complex products.
Can stability testing be shortened or simplified?
Yes, but only under specific conditions. ICH Q12 allows companies to use a risk-based approach for well-characterized drugs. If a product has a long history of stability data, minimal formulation changes, and proven degradation pathways, regulators may approve reduced testing frequency or shorter study durations. AI and predictive modeling are also being used to reduce sample sizes - but real-time data is still required for final expiration dates.
Why do stability chambers need such strict temperature control?
Even small changes in temperature or humidity can accelerate chemical degradation. A 5°C increase can double the rate at which a drug breaks down. Chambers are calibrated to ±2°C and ±5% RH to ensure results are reliable and reproducible. Temperature mapping studies are done quarterly to confirm every spot in the chamber performs the same. If one corner is 2°C warmer, it can invalidate months of data.
Is stability testing required for over-the-counter (OTC) drugs too?
Yes. OTC drugs like pain relievers, antacids, and allergy medications must meet the same ICH stability standards as prescription drugs. The FDA requires stability data for all active ingredients, regardless of whether a drug needs a prescription. The only difference is that OTC products often have simpler formulations, so testing may be less complex - but the requirements are just as strict.
sagar patel
December 26, 2025 AT 06:49Stability testing is the unsung hero of modern medicine
Bailey Adkison
December 26, 2025 AT 08:46They call it science but it's just regulatory theater. Most drugs are stable for decades. The 36-month requirement exists because regulators fear liability not because patients need it
Michael Dillon
December 27, 2025 AT 09:04Let's be real - if your aspirin doesn't work after two years you probably didn't store it right. But hey if Big Pharma wants to spend a million dollars per drug to prove it doesn't turn into poison I'm not stopping them
Gary Hartung
December 27, 2025 AT 12:22Do you realize the sheer audacity of assuming that a pill - a single, inert compound - can be trusted to remain chemically stable across wildly varying climates, humidity levels, and storage conditions? This isn't just testing. It's an act of faith in the precision of industrial chemistry. And yet, we're told to trust it. With our lives. Every. Single. Day.
Ben Harris
December 27, 2025 AT 23:50I used to work in a lab where they lost six months of data because someone left a door open during a heatwave. That's not science. That's a single human mistake costing millions. And they wonder why drugs cost so much
Carlos Narvaez
December 29, 2025 AT 05:41Biologics are the real challenge. A monoclonal antibody degrades faster than milk in summer. Stability testing for these isn't paperwork - it's survival engineering
Harbans Singh
December 29, 2025 AT 20:27Really interesting read. I'm from India and we don't always have perfect storage conditions. Do you think the same testing standards apply when medicines are shipped to places with no AC or reliable power?
Justin James
December 30, 2025 AT 19:25Did you know the FDA and pharma companies have a secret agreement? The real reason they don't extend expiration dates is because they want you to keep buying new bottles. They know most drugs last 5-10 years. But if you think your pills expire after 2 years you'll buy more. It's not about safety. It's about profit. The chambers? Just props. The data? Curated. The science? Manipulated
Rick Kimberly
January 1, 2026 AT 17:35While the cost of stability testing is substantial, the ethical imperative to ensure patient safety cannot be quantified in financial terms. The ICH Q1A(R2) framework represents a global consensus on the minimum acceptable standard for pharmaceutical integrity. Compromising this standard, even incrementally, undermines the foundational trust between the medical community and the public.
Terry Free
January 2, 2026 AT 19:30Oh wow. So we're spending millions to prove that aspirin doesn't turn into cyanide? How noble. Next they'll test my ibuprofen to make sure it doesn't magically become a spaceship
Lindsay Hensel
January 2, 2026 AT 21:15As someone who works in global health logistics, I've seen medicines stored in unrefrigerated huts and open-air markets. The gap between regulatory standards and real-world conditions is terrifying. We need better packaging, not just longer testing