Psoriasis as a Chronic Condition: Skin Care and Systemic Therapy Explained
 Dec, 10 2025
Dec, 10 2025
Psoriasis isn’t just a rash. It’s a full-body condition that starts on the skin but doesn’t stop there. For millions of people, it’s a lifelong battle - not just with flaky, red patches on elbows or scalp, but with joint pain, heart risks, depression, and the daily grind of managing something no cure can erase. If you or someone you know has psoriasis, you know it’s more than skincare. It’s about survival, control, and finding a rhythm that works when your body won’t cooperate.
What Psoriasis Really Is
Psoriasis is an autoimmune disease where your immune system accidentally attacks your own skin. Normally, skin cells take about 28 to 30 days to grow, die, and flake off. In psoriasis, that process speeds up to just 3 to 4 days. The cells pile up before they’re ready, forming thick, scaly plaques. These aren’t contagious. They’re not caused by poor hygiene. They’re a genetic signal gone wrong - with up to 90% of cases tied to family history. The most common type, plaque psoriasis, shows up as raised, red patches covered in silvery scales. You’ll often see them on knees, elbows, lower back, and scalp. But psoriasis doesn’t play by rules. Some people get inverse psoriasis - smooth, raw patches in skin folds like under the breasts or in the groin. Others develop pustules (sterile pus-filled bumps) on hands or feet. Rare but dangerous is erythrodermic psoriasis, where nearly the whole body turns red and inflamed, risking infection and fluid loss. It’s a medical emergency.It’s Not Just Skin Deep
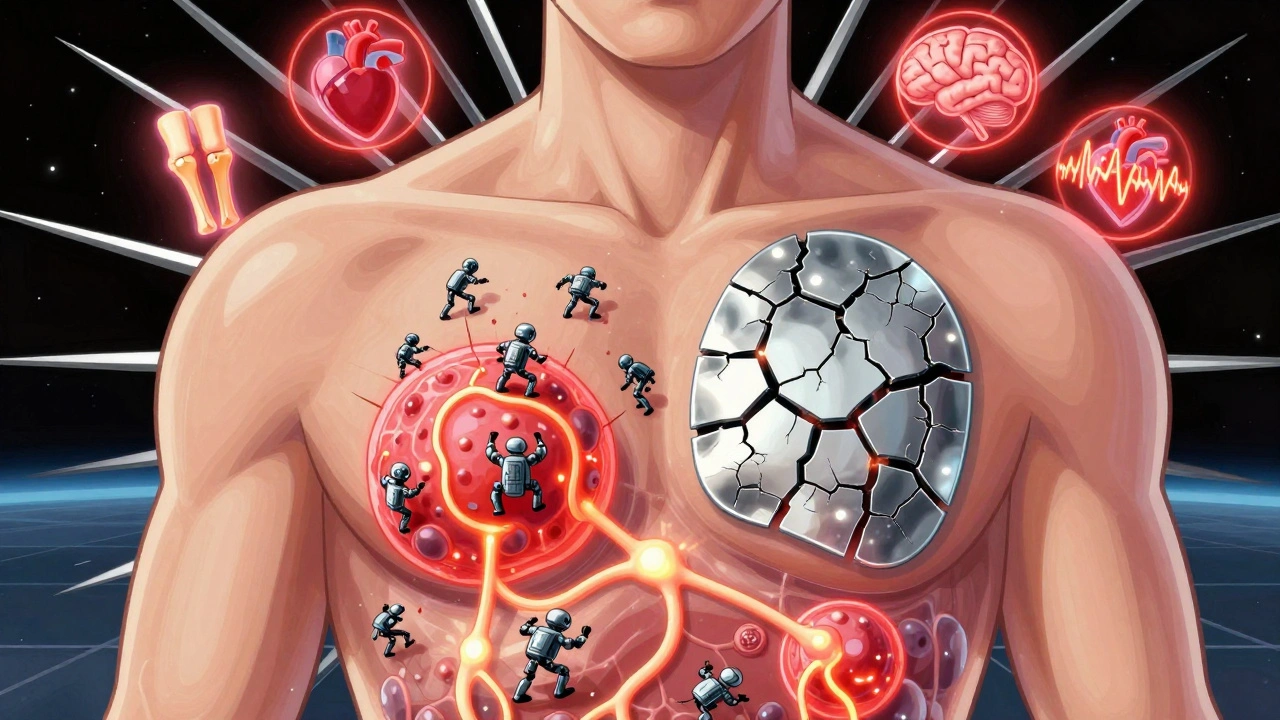
Here’s what most people don’t tell you: psoriasis is a systemic disease. That means it affects your whole body, not just your skin. About 30% of people with psoriasis develop psoriatic arthritis - joint pain, stiffness, swelling, often in fingers, toes, or spine. Nail changes like pitting, thickening, or separation from the nail bed are also common signs. The inflammation doesn’t stop at the joints. Studies show people with psoriasis have a 58% higher risk of heart attack before age 50. Nearly half have metabolic syndrome - high blood pressure, high blood sugar, excess belly fat, and abnormal cholesterol. Depression and anxiety are two to three times more common in psoriasis patients than in the general population. The constant visibility of the condition, the itching, the embarrassment - it wears you down. That’s why doctors now screen for more than skin. At every visit, you should get your blood pressure checked, your cholesterol tested, your BMI tracked, and your mood assessed. If your dermatologist isn’t asking about your heart or mental health, it’s time to find one who does.Topical Treatments: The First Line
Most people start with creams and ointments. Topical steroids reduce inflammation and itching. Vitamin D analogs like calcipotriol slow down skin cell growth. They’re often combined - like calcipotriol and betamethasone - to work faster and better. But they’re not magic. You have to use them consistently, and that’s hard. Scalp psoriasis? Foam or solution formulas work better than thick creams. Face and genitals? Avoid strong steroids. They can thin the skin. Instead, use mild vitamin D analogs or calcineurin inhibitors. For nails, topical treatments rarely help - injections or systemic drugs are needed. The biggest problem? Adherence. A 2023 survey on Reddit’s r/psoriasis found 67% of users struggled to apply topicals daily. They’re messy, time-consuming, and don’t always look like they’re working. Simplifying the routine - switching from twice-daily to once-daily regimens - can boost adherence by 40%, according to UCLA Health.
When Topicals Aren’t Enough: Phototherapy and Systemic Drugs
If creams don’t cut it, the next step is light therapy or pills. Narrowband UVB phototherapy is the most common. You go to a clinic 2-3 times a week for 8-12 weeks. It’s not fun, but it clears skin in 75% of cases. Home units cost $2,500-$5,000 upfront, plus monthly maintenance. Not everyone can afford that. Oral systemic drugs include methotrexate, cyclosporine, and acitretin. Methotrexate is a weekly pill that suppresses the immune system. It’s cheap but can hurt your liver and cause nausea. Cyclosporine works fast but can damage kidneys over time. Acitretin helps with pustular psoriasis but causes dry skin and birth defects - women must avoid pregnancy for three years after stopping. These aren’t first-choice drugs for mild cases. But for moderate to severe psoriasis, they’re often the bridge to biologics.Biologics: The Game Changers
Biologics are the most powerful tools we have today. They’re injectable or IV drugs that target specific parts of the immune system. Instead of shutting down your whole immune response, they hit just the troublemakers. TNF-alpha blockers like adalimumab (Humira) and etanercept (Enbrel) were the first. Then came IL-17 inhibitors like secukinumab (Cosentyx) and ixekizumab (Taltz), which clear skin faster. IL-23 inhibitors like guselkumab (Tremfya) and tildrakizumab (Ilumya) are newer - and often lead to near-complete clearance (PASI 90 or better) in over half of patients. Results? In clinical trials, secukinumab cleared 90% of plaques in 16 weeks for many. On Healthgrades, users rate biologics 4.3 out of 5 for effectiveness. But cost? That’s the wall. Monthly out-of-pocket costs can hit $1,200-$5,500 without good insurance. Even with coverage, copays can be $500-$1,000. Nearly half of patients skip or delay treatment because of price, according to the National Psoriasis Foundation. And it’s not just money. Injections are intimidating. You need training. Some people dread the needles. Others hate the idea of being “on biologics.” But for many, it’s the only way to get their life back.
The Treatment Gap and Why It Matters
Only 25-30% of people with moderate to severe psoriasis get systemic therapy. Why? Access. Rural areas have 40% fewer dermatologists per square mile than cities. Insurance hurdles delay approvals for months. Some doctors still think psoriasis is “just a skin issue.” The American Academy of Dermatology now pushes a “right-care-first” approach - matching treatment intensity to disease severity from day one. No more waiting for topicals to fail. If your skin covers 10% of your body and you’re in pain, you deserve biologics now. New guidelines (PCDS, January 2025) say your goal shouldn’t be “improved.” It should be near-clear or clear skin - PASI ≤3 and DLQI ≤4. That’s not a luxury. It’s the standard.Living With Psoriasis: Daily Habits That Help
No treatment works without daily care. Here’s what actually helps:- Moisturize daily - thick petrolatum-based ointments beat lotions. Apply right after showering.
- Use lukewarm water, not hot. Hot water dries you out and triggers flares.
- Choose gentle, fragrance-free cleansers. Avoid scrubbing.
- Identify triggers: stress, alcohol, smoking, infections, cold weather. Keep a symptom journal.
- Don’t pick or scratch. It can spread plaques (Koebner phenomenon).
- Quit smoking. It doubles your risk of severe psoriasis.
What’s Next? The Future of Psoriasis Care
New drugs are coming. Deucravacitinib (Sotyktu), a once-daily oral TYK2 inhibitor, cleared 58% of patients’ skin to PASI 90 in trials. Oral RORγt inhibitors are in Phase 2 - potentially replacing injections with pills. But the real shift is toward personalization. Researchers are mapping genetic profiles to predict which drug will work best for you. One person’s miracle drug might be another’s failure. Precision medicine isn’t sci-fi - it’s happening now. The challenge? Cost. Biologics make up 75% of the psoriasis market. Biosimilars help, but only cut prices by 15-30%. The system isn’t built for long-term, lifelong treatment. Still, the outlook is better than ever. Ten years ago, clearing 90% of skin was rare. Now, it’s the goal. You don’t have to live with plaques that ruin your confidence, your sleep, your relationships. There’s a path - and it starts with knowing you deserve more than a band-aid solution.Can psoriasis be cured?
No, psoriasis cannot be cured with current treatments. But it can be controlled. Many people achieve near-complete or complete skin clearance with biologics and consistent care. The goal is not just to reduce symptoms, but to restore quality of life.
Are biologics safe long-term?
Biologics are generally safe when monitored. They increase the risk of infections like tuberculosis, so screening is required before starting. Long-term data shows they don’t significantly raise cancer risk. Regular check-ups and blood tests help catch issues early. For most, the benefits far outweigh the risks.
Why do psoriasis treatments stop working?
The immune system can develop resistance to some biologics over time - especially TNF inhibitors. Switching to a different class, like an IL-17 or IL-23 inhibitor, often restores effectiveness. Other reasons include poor adherence, undiagnosed triggers (like stress or weight gain), or untreated comorbidities like obesity or diabetes.
Does stress make psoriasis worse?
Yes. Stress is one of the top triggers for flares. It activates the immune system, which worsens inflammation. Managing stress through mindfulness, therapy, exercise, or support groups can reduce flare frequency and severity. Some patients report fewer outbreaks after starting yoga or counseling.
Can diet help with psoriasis?
No diet cures psoriasis, but some changes help. Losing weight if overweight can improve symptoms - fat tissue produces inflammation. Cutting alcohol and processed sugars may reduce flares. Some find benefit in omega-3s (fish oil) or vitamin D supplements, though evidence is mixed. Always talk to your doctor before making big dietary changes.
What should I ask my dermatologist at my next visit?
Ask: What’s my PASI score? What’s my DLQI? Have my joints been checked for psoriatic arthritis? Are my blood pressure, cholesterol, and blood sugar being monitored? Am I on the right treatment for my severity? Is there a more affordable option? Don’t leave without clear answers.
Psoriasis doesn’t define you, but it does demand attention. The right care - skin care, systemic therapy, mental health support, and lifestyle changes - can turn a life of discomfort into one of control. You don’t have to accept flares as normal. There’s a better way, and it’s within reach.
Courtney Blake
December 12, 2025 AT 10:53Let me tell you something - this post is pure propaganda. Biologics are a scam run by Big Pharma to keep people hooked for life. You think you're getting better? Nah. You're just paying $5K a month to keep your skin from looking like a potato sack. And don't even get me started on the 'systemic' nonsense. Psoriasis is just a skin problem. Stop overmedicalizing it. Get a good moisturizer and quit whining.
Also, why are we letting insurance companies dictate our treatment? If you can't afford it, tough luck. That's America. 💩
Lisa Stringfellow
December 13, 2025 AT 22:05Ugh. Another one of those 'psoriasis is an autoimmune disease' lectures. I've seen this exact post three times on Reddit. Someone just copy-pasted a medical textbook and called it 'insight.'
Also, why do you keep saying 'you deserve better'? Who are you, a therapist? I just want to know if coconut oil works. That's it. No lectures. No PASI scores. Just tell me if it works or not.
Also, the author sounds like they're getting paid by Humira. 🙄
Kristi Pope
December 15, 2025 AT 21:02Hey - I just want to say thank you for writing this. I’ve had psoriasis for 18 years and no one’s ever explained it like this before. I used to think I was broken. Now I know my body’s just fighting a war I didn’t ask for.
And to everyone saying ‘just use coconut oil’ - I’ve tried it. I’ve tried everything. The real win isn’t clearing 90% of plaques - it’s being able to wear a tank top again without feeling like a monster.
You’re not alone. Seriously. I’m here. We’re all here. 🌱
Aman deep
December 16, 2025 AT 12:14thank you for this post i live in india and we dont have access to biologics at all here my derm says try steroids and hope for the best
but i read about your post and i feel seen for the first time. i dont know if i can afford even a monthly visit but knowing that someone out there gets it… it helps
ps. i use shea butter and lukewarm showers and it helps a little. not perfect but better than nothing. 🙏
Eddie Bennett
December 16, 2025 AT 20:44Big fan of the post. Real talk - most dermatologists treat psoriasis like it’s a cosmetic issue. I had a doc tell me to ‘just stop stressing’ while I was crying in the exam room. That’s not care. That’s dismissal.
Biologics saved my life. I used to wear long sleeves in 95-degree heat. Now I wear shorts. That’s not a win - that’s freedom.
And yeah, they’re expensive. But if your insurance denies you, fight back. Call your state’s patient advocate office. They’ll help. I did. Took 6 months. Worth it.
Sylvia Frenzel
December 18, 2025 AT 04:13Oh please. You’re telling people to get biologics like they’re Starbucks lattes. Did you even check the side effects? My cousin got liver failure from methotrexate. Now she’s on a transplant list. And you want me to just ‘switch to IL-23 inhibitors’ like it’s a Netflix subscription?
This isn’t healthcare. It’s a lottery. And most of us are stuck with the losing ticket. 🤷♀️
Vivian Amadi
December 19, 2025 AT 23:34You’re wrong. Psoriasis is caused by gluten. Stop lying. Cut out bread. Done. No injections needed. I cured mine in 3 weeks. You’re all just too lazy to try.
john damon
December 20, 2025 AT 19:22Just wanted to say I’m 3 months into Humira and my skin looks like a newborn’s. I cried the first time I saw my elbows without scales. 🥹
Also, the cost is insane but my insurance covered 90%. If you’re struggling - DM me. I’ll help you navigate the paperwork. No one should suffer alone.