OTC Antacids and Antibiotics: How They Reduce Absorption and Risk Treatment Failure
 Nov, 16 2025
Nov, 16 2025
Antacid-Antibiotic Timing Calculator
How This Calculator Works
Many antacids contain metal ions (aluminum, magnesium, calcium) that can bind to antibiotics in your gut. This calculator shows the safe time gaps to prevent reduced antibiotic effectiveness. Always follow your doctor's specific instructions.
Important Notes
For fluoroquinolones (ciprofloxacin, levofloxacin): Minimum 4-6 hours gap is critical. Less than 4 hours significantly reduces effectiveness.
For tetracyclines (doxycycline): Minimum 2 hours before or 4 hours after antacid.
Even small gaps can matter—don't guess the timing. Use a timer or alarm.
One accidental overlap won't ruin treatment, but repeated timing errors can lead to treatment failure.
Many people reach for an OTC antacid like Tums, Maalox, or Mylanta when they feel heartburn or indigestion. It’s fast, easy, and works right away. But if you’re also taking an antibiotic-maybe for a sinus infection, urinary tract infection, or pneumonia-you could be making your treatment less effective without even knowing it. This isn’t just a small risk. It’s a well-documented, clinically significant interaction that can lead to treatment failure, longer illness, and even antibiotic resistance.
Why Antacids Interfere with Antibiotics
The problem isn’t that antacids are dangerous on their own. They’re designed to neutralize stomach acid using metal ions like aluminum, magnesium, and calcium. These same metal ions bind tightly to certain antibiotics in your gut, forming what’s called a chelate complex. Think of it like a magnet sticking to metal. Once that bond forms, the antibiotic can’t be absorbed into your bloodstream the way it should. Instead, it passes through your system mostly unchanged. This isn’t true for all antibiotics. The big offenders are tetracyclines (like doxycycline) and fluoroquinolones (like ciprofloxacin and levofloxacin). Studies show that when taken with aluminum- or magnesium-containing antacids, tetracycline absorption can drop by 70% to 90%. For ciprofloxacin, bioavailability can fall from 70% to as low as 15%. That means you’re getting a fraction of the dose you paid for. Even amoxicillin, a commonly prescribed penicillin-type antibiotic, isn’t completely safe. One study found its absorption dropped by 18-22% when taken with common antacids like Maalox. That might not sound like much, but in an infection fighting for every advantage, even a 20% drop can tip the scales.Which Antacids Are the Worst?
Not all antacids are created equal. The ones with aluminum hydroxide, magnesium hydroxide, or calcium carbonate are the biggest culprits. Here’s what you’re likely to find in your medicine cabinet:- Tums (calcium carbonate): Often used for quick relief, but calcium binds strongly with fluoroquinolones.
- Maalox and Mylanta (aluminum + magnesium hydroxide): These are among the most problematic because they combine two binding agents.
- Rolaids (calcium carbonate + magnesium hydroxide): Same issue-two metal ions working together to block absorption.
- Alka-Seltzer (sodium bicarbonate): Less binding, but still alters stomach pH enough to affect some antibiotics.
How Much Does This Actually Affect Treatment?
It’s not theoretical. Real patients fail antibiotic courses because of this. A 2024 case study from University Hospitals described a woman with recurring UTIs. She took ciprofloxacin as prescribed, but also chewed Tums daily for acid reflux. Her infections kept coming back. Cultures showed the same bacteria each time. Only after she stopped taking Tums within hours of her antibiotic did her symptoms clear up-and her urine cultures turned negative. A 2023 meta-analysis found that people who took antacids at the same time as antibiotics had a 37% higher chance of treatment failure compared to those who spaced them out. That’s not a small number. It means nearly 4 out of 10 people might not get better because of something as simple as timing. And it’s not just about not feeling better. When antibiotics don’t work, bacteria survive. Surviving bacteria are the ones that evolve. They become resistant. That’s how we get superbugs. The CDC estimates over 35,000 deaths in the U.S. each year are linked to antibiotic-resistant infections. Every time a course fails due to poor timing, we add to that number.
What About Other Acid Reducers?
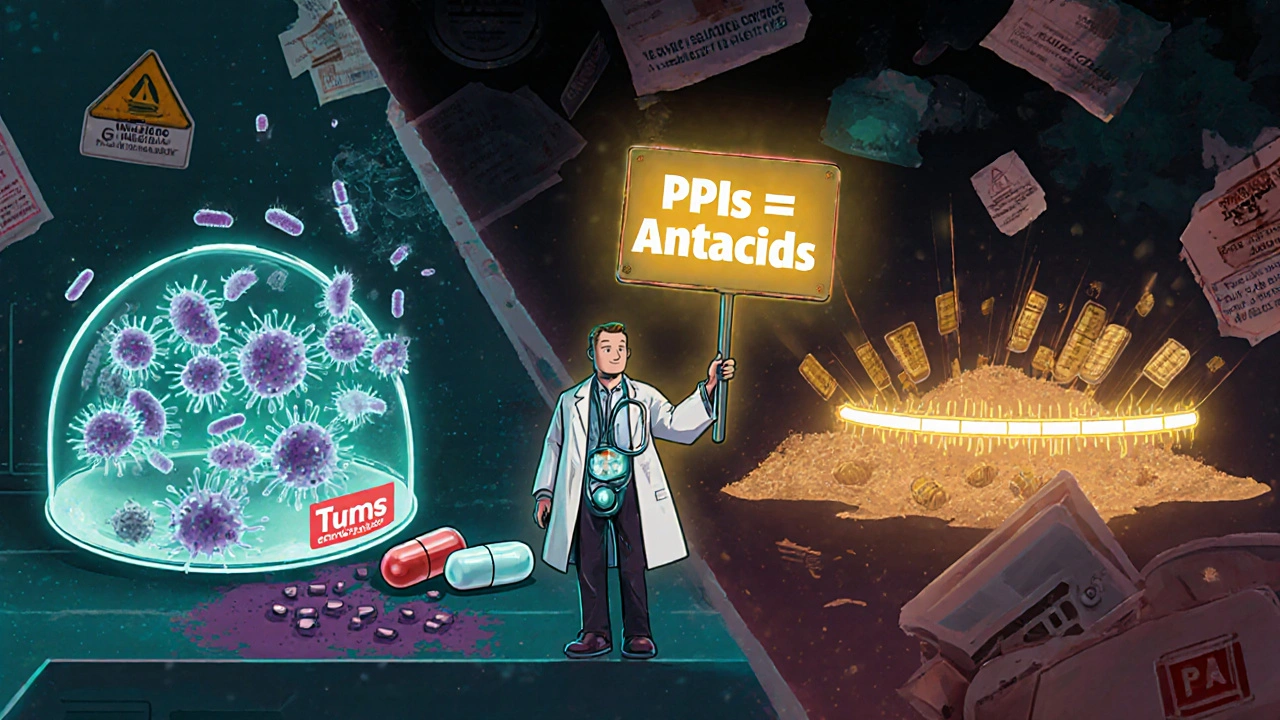
You might be thinking: “What if I use famotidine (Pepcid) or omeprazole (Prilosec) instead?” Those are safer options. H2 blockers and proton pump inhibitors (PPIs) work differently. They don’t contain metal ions. Instead, they reduce acid production at the source. That means no chelation. No binding. No direct interference with antibiotic absorption. But here’s the catch: they don’t work as fast. Antacids relieve symptoms in 1-5 minutes. PPIs take 1-4 hours. H2 blockers take 30-60 minutes. So if you’re in pain right now, antacids feel like the obvious choice. The trade-off is real. If you need immediate relief while on antibiotics, switching to a PPI or H2 blocker is the smarter move-even if it takes longer to kick in. It’s not about comfort. It’s about making sure your antibiotic actually works.How to Take Them Correctly
Timing isn’t optional. It’s the difference between success and failure. Here’s what the experts recommend:- For tetracyclines (doxycycline, minocycline): Take the antibiotic at least 2 hours before or 4 hours after the antacid.
- For fluoroquinolones (ciprofloxacin, levofloxacin): Wait 4 to 6 hours after taking the antacid before taking your antibiotic. Or take the antibiotic first, then wait 4-6 hours before the antacid.
- For amoxicillin: While the effect is smaller, it’s still worth spacing them by at least 2 hours if you’re on a high-dose regimen or have a serious infection.
Who’s at Highest Risk?
This isn’t just a “be careful” warning. Some people are way more likely to run into this problem:- Elderly patients: More likely to take multiple medications, including antacids for acid reflux, and less likely to be warned about interactions.
- People with chronic reflux: Those who take antacids daily or multiple times a day.
- Patients on long-term antibiotics: Like those treating bone infections or chronic bronchitis.
- People who self-medicate: Those who grab antacids without telling their doctor or pharmacist.
What Should You Do?
If you’re prescribed an antibiotic:- Ask your pharmacist: Right when you pick up your prescription. Say: “I take antacids for heartburn. Will this interfere?”
- Check the label: Look for “Do not take with antacids” or “Separate doses by 2-4 hours.”
- Switch to a safer acid reducer: If you need daily acid control, ask your doctor about famotidine or a low-dose PPI for the duration of your antibiotic course.
- Don’t guess the timing: Use a timer or app to space doses correctly. Two hours isn’t enough for ciprofloxacin. Four hours isn’t enough for doxycycline if you’re also taking a high-dose antacid.
The Bigger Picture
The OTC antacid market is worth over $2.8 billion. Millions of people use them every week. Antibiotics are prescribed over 250 million times a year in the U.S. alone. That’s a lot of overlap. The FDA required labeling changes in 2019 to warn about this interaction. But by 2022, only 67% of major brands fully complied. That means nearly a third of the bottles you buy still don’t say it clearly enough. Pharmacists are on the front lines. They’re the ones who see you walk in for your antibiotic and then buy Tums right next to the register. They’re trained to catch this. But they can’t read your mind. You have to speak up. This isn’t just about avoiding discomfort. It’s about making sure your antibiotics work. It’s about stopping the spread of resistance. It’s about not having to go through another round of sickness because you didn’t know how to time your pills.What If You’re Already on Both?
If you’re currently taking antibiotics and antacids together, here’s what to do now:- Stop taking them at the same time-immediately.
- Set alarms to space them correctly.
- Call your pharmacy and ask: “What’s the safest way to take my antibiotic with my antacid?”
- If you’re still not feeling better after 2-3 days, contact your doctor. You might need a different antibiotic or a different approach.
Can I take antacids and antibiotics at the same time if I chew them?
No. Chewing antacids doesn’t change how they interact with antibiotics. Whether you swallow a tablet or chew a tablet, the metal ions (aluminum, magnesium, calcium) still bind to the antibiotic in your stomach and intestines. The only thing that matters is timing-how far apart you take them. Chewing might make the antacid work faster, but it doesn’t make the interaction any less dangerous.
Does it matter if I take the antacid before or after the antibiotic?
Yes. For most antibiotics like doxycycline and ciprofloxacin, taking the antibiotic first and waiting 4-6 hours before the antacid is safest. That way, the antibiotic has time to be absorbed before the antacid alters your gut environment. If you take the antacid first, you’re creating a binding environment before the antibiotic even arrives. That’s when absorption drops the most.
Are all antacids equally bad with antibiotics?
No. Antacids with aluminum hydroxide, magnesium hydroxide, or calcium carbonate are the worst. Sodium bicarbonate (like Alka-Seltzer) has less binding power but still changes stomach pH, which can affect some antibiotics. Antacids with only simethicone (for gas) don’t cause this issue-but they’re rarely sold alone. Always check the active ingredients on the label.
What if I only took one antacid by accident?
One accidental dose is unlikely to ruin your treatment. But if you’ve done this multiple times over a few days, it could lower your antibiotic levels enough to let bacteria survive. If you’re still having symptoms after a couple of days, contact your doctor. You might need a repeat test or a different antibiotic.
Can I use baking soda instead of antacids?
Baking soda (sodium bicarbonate) is an antacid too. It’s less likely to bind with antibiotics than aluminum or magnesium, but it still raises stomach pH. This can reduce absorption of some antibiotics, especially tetracyclines. It’s not a safer alternative-it’s just a different kind of risk. Stick to spacing or switch to famotidine or omeprazole if you need daily acid control.
Joseph Townsend
November 17, 2025 AT 15:43Bro. I took Tums with my doxycycline for three days straight because I thought heartburn was just ‘part of being sick.’ Turns out I was just feeding my sinus infection a VIP pass to survive. Now I’m back on round two. Don’t be me. Space your pills. Your future self will thank you. 🤦♂️
Bill Machi
November 19, 2025 AT 14:37This is why America is falling apart. People swallow antacids like candy and then wonder why their antibiotics don’t work. No one reads labels anymore. No one takes responsibility. The FDA warned you. The pharmacist warned you. Your own damn bottle warned you. And yet-you still chow down Tums like they’re M&Ms. This isn’t ignorance. It’s willful negligence. And it’s killing us.
Elia DOnald Maluleke
November 20, 2025 AT 10:39It is not merely a pharmacological interaction-it is a metaphysical rupture in the human relationship with self-care. We have reduced medicine to a transaction: quick fix for discomfort, blind obedience to convenience. The metal ions bind not only to antibiotics but to our very capacity for foresight. In chewing Tums, we chew away the future. The bacteria, ever patient, inherit the earth-not through virulence, but through our collective apathy.
satya pradeep
November 21, 2025 AT 03:04bro i was literally doing this till last week 😅 i took cipro + maalox together because i was cramping after dinner. then i got dizzy and the infection came back. called my pharma guy-he laughed and said ‘dude, you’re basically giving your bacteria a vacation.’ now i set alarms. 4 hours apart. life changed. also, switch to pepcid if you’re on antibiotics long-term. saves your sanity.
Prem Hungry
November 22, 2025 AT 11:54Dear friend, let me offer you a gentle but firm reminder: your health is not a suggestion-it is a sacred covenant with your body. While OTC antacids provide momentary relief, they do so at the cost of your systemic integrity. The bioavailability of antibiotics is not a statistical abstraction; it is the difference between recovery and relapse. I urge you, with all sincerity, to consult your pharmacist, to mark your calendar, and to prioritize healing over comfort. Your resilience is worth the wait.
Leslie Douglas-Churchwell
November 24, 2025 AT 04:29Okay but have you considered this is a Big Pharma psyop? 🤔 Tums is owned by Johnson & Johnson-who also own antibiotic manufacturers. They want you to take BOTH so you need MORE antibiotics later. That’s why the warning labels are buried under 8-point font. Also, the CDC? Controlled by the WHO. And WHO? Funded by Gates. They want antibiotic resistance to drive the ‘next-gen’ vaccine rollout. I stopped taking antibiotics entirely and now I use colloidal silver + lemon water. My UTI cleared in 2 days. Coincidence? I think not. 💉🫠
shubham seth
November 25, 2025 AT 15:12Let’s be real-this whole post is just a glorified pharmacy ad disguised as public health. You didn’t mention that PPIs increase the risk of C. diff, pneumonia, and bone loss. You didn’t mention that 60% of people on long-term PPIs develop B12 deficiency. You just said ‘switch to Pepcid’ like it’s a magic bullet. Meanwhile, your solution creates five new problems. We’re treating symptoms like they’re enemies, not signals. This isn’t medicine. It’s corporate triage wrapped in a white coat.
Kathryn Ware
November 27, 2025 AT 02:09I’m so glad someone finally wrote this. I’m a nurse and I see this EVERY WEEK. A 72-year-old woman comes in with a UTI, takes cipro, and then chews 4 Tums because her reflux is ‘acting up.’ She doesn’t even know they’re interacting. I’ve had to call doctors to change antibiotics because the culture came back positive again. I keep little printed cards in my bag-‘Antibiotic + Antacid Timing Cheat Sheet’-and hand them out. Seriously, set a phone alarm. Write it on your hand. Tell your spouse. This isn’t complicated, but it’s life-or-death. And if you’re on amoxicillin and think ‘it’s just a 20% drop’-trust me, in a stubborn infection, that’s the difference between going to work and being in the hospital. You’re not being dramatic. You’re being smart. ❤️🩺