Opioids and Sleep Apnea: How Opioids Trigger Dangerous Breathing Problems During Sleep
 Nov, 4 2025
Nov, 4 2025
Opioid Sleep Apnea Risk Calculator
Risk Assessment
Enter your opioid dose and other factors to calculate your risk level
Risk Results
Recommended Actions
- Get a sleep study
- Consider CPAP therapy
- Discuss dose reduction with your doctor
When you take opioids for pain, you’re not just managing discomfort-you’re also putting your breathing at risk, especially while you sleep. This isn’t a rare side effect. It’s a life-threatening interaction that affects tens of thousands of people every year. If you or someone you know is on long-term opioid therapy and snores, wakes up gasping, or feels exhausted even after a full night’s rest, the problem might not be just poor sleep-it could be opioid-induced respiratory depression.
How Opioids Quiet Your Breathing
Opioids like oxycodone, morphine, fentanyl, and hydrocodone work by binding to receptors in your brain that control pain. But they don’t stop there. The same receptors are found in the brainstem-the part of your brain that automatically controls breathing. When opioids activate these receptors, they slow down the signals that tell your lungs to inhale and exhale. This isn’t just a slight reduction in breaths per minute. It’s a dangerous suppression that can lead to pauses in breathing called apneas, sometimes lasting 20 seconds or longer. Research shows that opioids reduce respiratory rate by making exhalation last much longer than normal-up to double or even triple the usual time. At the same time, they weaken the muscles that keep your airway open during sleep, especially the tongue and throat muscles. This combination-slowed breathing plus collapsed airways-is what turns ordinary sleep apnea into something far more dangerous.The Brain Regions That Opioids Target
Two key areas in the brainstem are hit hardest: the pre-Bötzinger complex and the parabrachial complex. The pre-Bötzinger complex controls the rhythm of breathing. The parabrachial complex, especially the Kölliker-Fuse nucleus, acts like a safety switch that prevents you from stopping breathing entirely. When opioids hit the parabrachial complex, they disable this safety mechanism. Studies in mice show that removing opioid receptors from this area reduces life-threatening apneas by up to 80%. What’s alarming is that the pre-Bötzinger complex only helps at low, pain-relieving doses. Once the dose increases-even slightly-this area can’t compensate anymore. The parabrachial complex is the real gatekeeper. If it’s suppressed, breathing can stop completely, even if you’re not overdosing in the traditional sense.Why Sleep Makes It Worse
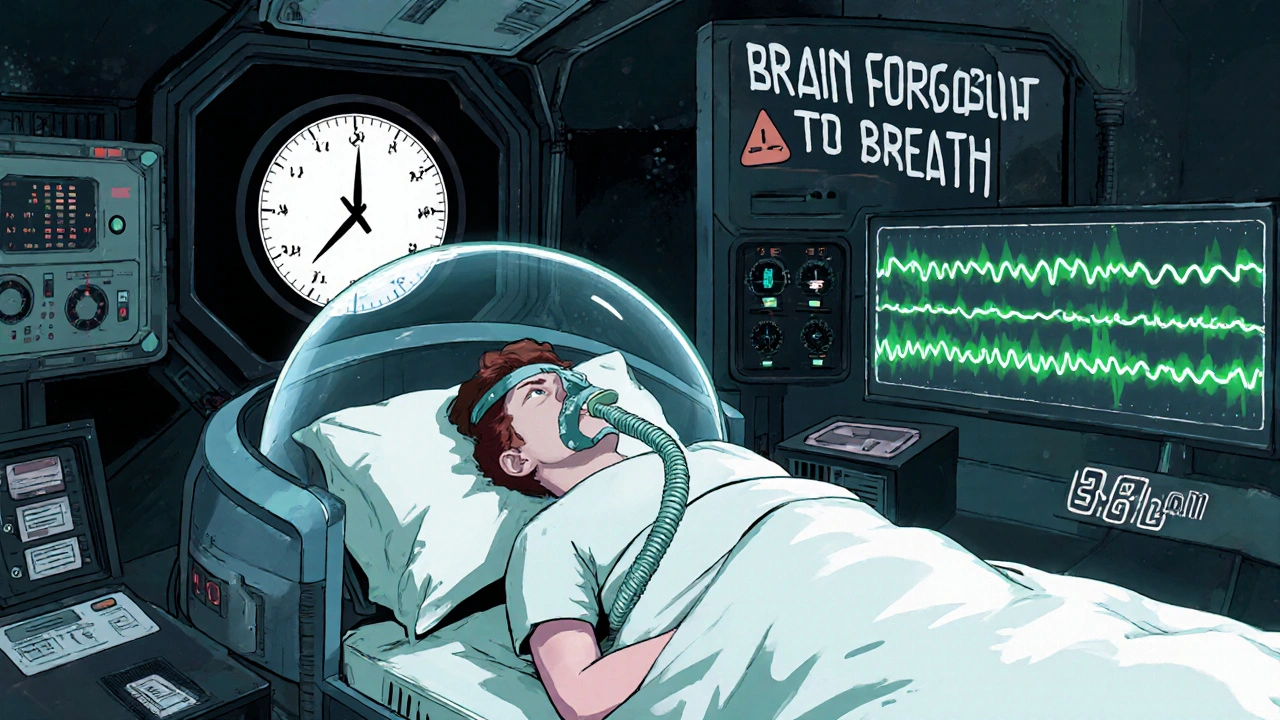
During wakefulness, your brain sends extra signals to keep breathing steady, even if opioids are present. But when you fall asleep, those signals fade. That’s when opioids take full control. The result? Central sleep apnea-where your brain simply forgets to tell your lungs to breathe. People on high-dose opioids (100 morphine milligram equivalents or more per day) have an average of 15 to 16 breathing pauses per hour. That’s the level seen in severe sleep apnea. Some patients hit 30 or more. Opioids also mess with your sleep stages. They reduce deep, restorative slow-wave sleep by 20-30% and increase light, unstable sleep. This means even if you sleep for eight hours, your body never gets the recovery it needs. Waking up tired, with headaches or a dry mouth, isn’t just “bad sleep”-it’s a sign your body struggled to breathe all night.Who’s at Highest Risk?
Not everyone on opioids develops this problem, but certain factors make it much more likely:- Already having obstructive sleep apnea before starting opioids
- Taking doses above 50 morphine milligram equivalents per day
- Using opioids with benzodiazepines, alcohol, or sleep aids
- Being over 65 or having heart or lung disease
- Having a genetic variation in the OPRM1 gene, which affects how opioids bind to receptors
The Silent Danger: Normal Oxygen Levels Can Be Misleading
A pulse oximeter showing 95% oxygen saturation might make you feel safe. But that number can stay normal even when breathing is dangerously slow. Why? Because your body compensates by taking deeper breaths between pauses. By the time oxygen drops, it’s often too late. Capnography-which measures carbon dioxide levels-is far more reliable for detecting early respiratory depression. Yet, only 15-20% of primary care providers screen for it in opioid patients.What Happens When Opioids Mix With Other Depressants
Combining opioids with benzodiazepines (like Xanax or Valium), alcohol, or even some over-the-counter sleep medications multiplies the danger. The CDC reports that this combination increases the risk of fatal overdose by 300-500%. It’s not just additive-it’s exponential. Both types of drugs suppress the brainstem. Together, they can shut down breathing completely, even at doses that are safe on their own.What Can Be Done?
If you’re on opioids and suspect you might have sleep apnea, don’t wait for symptoms to get worse. Here’s what works:- Get a sleep study. A home or lab-based polysomnography can detect central apnea caused by opioids. This is especially important if you’ve been on opioids for more than three months.
- Ask about CPAP. Continuous Positive Airway Pressure machines are standard for obstructive sleep apnea. But for central apnea caused by opioids, they can still help by keeping airways open and stimulating breathing.
- Check your dose. If you’re on more than 50 morphine milligram equivalents per day, talk to your doctor about tapering or switching to a non-opioid pain management plan.
- Keep naloxone on hand. Naloxone reverses opioid overdose. It’s not just for heroin users-anyone on long-term opioids should have it available. A nasal spray like Narcan can save a life while waiting for emergency help.
- Avoid alcohol and sedatives. Even one drink at night can push you over the edge.

What’s Coming Next?
Scientists are working on next-generation opioids that relieve pain without suppressing breathing. Early lab compounds, called “biased agonists,” activate pain pathways but leave respiratory pathways mostly untouched. In animal studies, they’ve shown 70-80% pain relief with only 20-30% respiratory depression. That’s a huge leap. The NIH has invested $1.5 billion into finding safer pain treatments. In the next five years, genetic testing may become routine to identify people at high risk for opioid-induced respiratory depression before they ever take a pill. For now, awareness and screening are your best defenses.Real Stories, Real Consequences
Online patient forums are filled with posts like: “I wake up gasping every night since I started my pain meds.” “My wife says I stop breathing for 10 seconds at a time.” “I thought it was just bad dreams-turns out it was my brain shutting off.” These aren’t isolated cases. They’re symptoms of a widespread, underdiagnosed crisis. One study found that 65% of opioid users reporting sleep breathing problems described waking up terrified, unable to catch their breath. Many assumed it was anxiety. Others thought they were just getting older. The truth? Their brain had been silenced by medication.Don’t Assume It’s Just ‘Normal’
If you’re on opioids and your sleep feels off-whether you snore, wake up tired, have headaches, or feel like you’re not getting enough air-don’t brush it off. This isn’t something you have to live with. It’s a medical issue with real solutions. The sooner you talk to your doctor, the safer you’ll be.Can opioids cause central sleep apnea?
Yes. Opioids suppress the brainstem’s ability to signal breathing during sleep, leading to central sleep apnea-where breathing stops because the brain doesn’t send the signal to start. This is different from obstructive sleep apnea, where the airway is blocked. Opioid-induced central apnea is common in long-term users and can be severe, with 15-30 breathing pauses per hour.
Is it safe to take opioids if I already have sleep apnea?
It’s risky. Having untreated sleep apnea before starting opioids greatly increases your chance of life-threatening breathing problems. If you have sleep apnea and need opioids, your doctor should first treat the apnea-with CPAP or another therapy-and then carefully monitor your opioid dose. Never start opioids without a sleep study if you have known sleep apnea.
How do I know if my opioids are affecting my breathing at night?
Look for these signs: waking up gasping or choking, morning headaches, dry mouth, excessive daytime sleepiness, unrefreshing sleep, or being told by a partner that you stop breathing during sleep. If you have any of these and are on opioids, ask your doctor for a sleep study. Don’t wait for an emergency.
Can naloxone reverse opioid-induced sleep apnea?
Naloxone can reverse opioid-induced respiratory depression during an overdose, including breathing pauses caused by opioids. It works by blocking opioid receptors in the brainstem. However, it’s not a long-term solution. It doesn’t treat the underlying apnea, and repeated use can trigger withdrawal. Keep naloxone on hand if you’re on high-dose opioids, but focus on prevention through sleep screening and dose management.
Are there safer alternatives to opioids for chronic pain?
Yes. Non-opioid options include physical therapy, cognitive behavioral therapy, NSAIDs (like ibuprofen or naproxen), gabapentin for nerve pain, and certain antidepressants. For severe pain, procedures like nerve blocks or spinal cord stimulation may help. Newer non-addictive pain medications are in development, and many patients find relief through multi-disciplinary pain clinics that avoid opioids entirely.
Alex Harrison
November 6, 2025 AT 12:10I never realized how much opioids mess with your breathing at night. I’ve been on them for two years for my back pain and I wake up gasping all the time. Thought it was just stress or old age. Guess I need to get a sleep study ASAP.
Jay Wallace
November 7, 2025 AT 09:22Of course the government wants to ban opioids-because they’re too easy to abuse. But what about people who actually need them? This article reads like propaganda from the anti-pill crowd. If you can’t handle a little respiratory depression, maybe you shouldn’t be on pain meds at all.
Alyssa Fisher
November 8, 2025 AT 17:40It’s fascinating how the brainstem has these built-in fail-safes-like the parabrachial complex-and opioids just disable them like a switch. It’s not just about addiction; it’s about the body’s most basic functions being hijacked. We treat pain like a simple problem to solve, but the brain doesn’t work that way. There’s a cost. And most people don’t even know they’re paying it.
Alyssa Salazar
November 8, 2025 AT 22:02Let’s be real-this is a public health disaster in slow motion. Opioid-induced central apnea isn’t rare, it’s epidemic. And yet, primary care docs are still relying on pulse oximeters like they’re gospel. Capnography is the gold standard, and 80% of providers don’t even know what it is. We need mandatory screening protocols. This isn’t optional-it’s life-or-death.
Beth Banham
November 10, 2025 AT 11:54I’ve got a friend on high-dose oxycodone. She never mentioned any breathing issues until I asked if she ever woke up feeling like she couldn’t breathe. She said yes, every night. She thought it was normal. I’m so glad this article exists. People need to know this isn’t just ‘bad sleep.’
Brierly Davis
November 12, 2025 AT 07:18Hey, if you’re on opioids and snoring or waking up tired, don’t ignore it. Get tested. Get a CPAP if needed. Keep naloxone in your medicine cabinet. You’re not weak for needing help-you’re smart for asking for it. I’ve seen too many people lose their lives because they thought it was ‘just how it is.’ You deserve better.
Amber O'Sullivan
November 13, 2025 AT 01:08Jim Oliver
November 13, 2025 AT 08:00So let me get this straight: people are too lazy to stop taking opioids, so now we need to screen them for breathing problems? And we’re supposed to feel bad for them? Wake up. If you can’t manage your own health, don’t blame the medicine. Naloxone isn’t a free pass-it’s a bandage on a gunshot wound.
William Priest
November 14, 2025 AT 02:40Biased agonists? That’s the future? Sounds like science fiction. The real solution is stopping opioid prescriptions cold turkey. No more ‘safe’ opioids-because there’s no such thing. If you want pain relief, go to a chiropractor. Or yoga. Or cry about it. But don’t poison your brainstem for convenience.
Ryan Masuga
November 15, 2025 AT 23:43I was on 120 MME for years after my surgery. Woke up every morning with a headache and felt like I’d been run over. My wife said I stopped breathing. I thought it was just stress. Got a sleep study, turned out I had 28 apneas an hour. Switched to gabapentin and physical therapy. I haven’t felt this good in 5 years. You don’t have to suffer. There’s another way.
Jennifer Bedrosian
November 16, 2025 AT 21:45OMG I thought I was going crazy!! I’ve been on hydrocodone for 3 years and I wake up terrified like I’m drowning. My husband says I turn blue. I thought it was anxiety or PTSD. I just cried reading this. I’m calling my doctor tomorrow. I’m not alone. Thank you for saying this out loud.
Lashonda Rene
November 17, 2025 AT 01:02I think people need to understand that pain is real and opioids help but they also mess with your body in ways you can’t see. Like your brain forgets to breathe. It’s not your fault. It’s not weak. It’s just how the medicine works. And if you’re scared to talk to your doctor, just know that you’re not the only one. I didn’t know any of this until my mom had a scare. Now I tell everyone I know. Just get checked. It’s not a big deal. It’s just a sleep test. It could save your life.
Andy Slack
November 18, 2025 AT 18:54One sentence: If you’re on opioids and sleep is off, get tested. Now.