Healthcare Communication Training: How Institutional Education Programs Improve Patient Outcomes
 Dec, 5 2025
Dec, 5 2025
When patients leave the doctor’s office confused, or when nurses and doctors miscommunicate about a treatment plan, the consequences aren’t just frustrating-they’re dangerous. Studies show that healthcare communication failures contribute to 80% of serious medical errors, according to The Joint Commission. Yet most hospitals still treat communication as an afterthought, not a core skill. That’s changing. Across the U.S., institutional generic education programs are being rolled out to fix this broken system-not with slogans, but with real, evidence-based training that’s saving lives, reducing lawsuits, and rebuilding trust.
Why Communication Training Isn’t Optional Anymore
It’s not enough to say, "Be nice to patients." That’s not training. Real communication training teaches specific behaviors that change outcomes. For example, a physician who learns to ask, "What’s your biggest concern right now?" instead of jumping to diagnosis sees patients who are 40% more likely to follow their treatment plan. That’s not magic-it’s data. A 2022 study from Press Ganey found a 0.78 correlation between communication quality and patient satisfaction scores. That’s stronger than the link between pain medication and pain relief. The financial stakes are just as high. Hospitals with trained staff see 30% fewer malpractice claims, according to Johns Hopkins Medicine. Why? Because patients who feel heard don’t sue. They trust. And when staff communicate clearly with each other, medication errors drop by up to 25%. The Affordable Care Act and Medicare now tie 30% of hospital reimbursements to patient-reported communication scores (HCAHPS). If your staff can’t communicate, your hospital loses money.What These Programs Actually Teach
These aren’t one-hour webinars. They’re structured, multi-week programs built on decades of research. The Program for Excellence in Patient-Centered Communication (PEP) at the University of Maryland, for example, trains clinicians in five core skills: eliciting the patient’s story, recognizing emotional cues, responding with empathy, negotiating treatment plans, and closing the loop with clear next steps. Each skill is practiced with standardized patients-actors trained to mimic real medical scenarios. At Mayo Clinic, nurses take a 3.5-credit online course that includes 12 real-life video demonstrations. One module shows how to set boundaries with demanding family members. Another teaches how to read non-verbal cues-like a patient who says "I’m fine" but won’t make eye contact. These aren’t theoretical. They’re tools used daily in ERs, clinics, and ICUs. Meanwhile, Northwestern University uses mastery learning: students must hit 85% proficiency on communication assessments before moving on. They do 4 to 6 simulated sessions during clinical rotations. The result? 37% higher skill retention after six months compared to traditional lectures. That’s because they’re not memorizing scripts-they’re rewiring how they interact.Programs for Different Roles, Different Needs
Not all communication training is the same. Some are designed for frontline staff. Others target leaders. The Society for Healthcare Epidemiology of America (SHEA) offers a $75-$125 course for infection control specialists. It covers how to talk to the media during an outbreak, how to write public health advisories, and how to use social media to correct vaccine misinformation. One participant from Cleveland Clinic said her training helped her reach 50,000 people with accurate info-directly countering viral falsehoods. The University of Texas at Austin’s Health Communication Training Series (HCTS) is free and focuses on public health emergencies. Launched in 2022, it teaches hospitals how to coordinate messaging during pandemics. The CDC found that 40% of early pandemic delays were due to poor internal communication. HCTS was built to fix that. For administrators and policy makers, master’s programs like Johns Hopkins’ Online MA in Communication with Health Concentration offer deeper theory. It’s a 30-credit program costing $1,870 per credit. Students study health disparities, media framing, and policy advocacy. But here’s the catch: while these programs build expertise, they don’t always translate to the bedside. That’s why most hospitals now combine both-short, practical training for staff, and advanced degrees for leadership.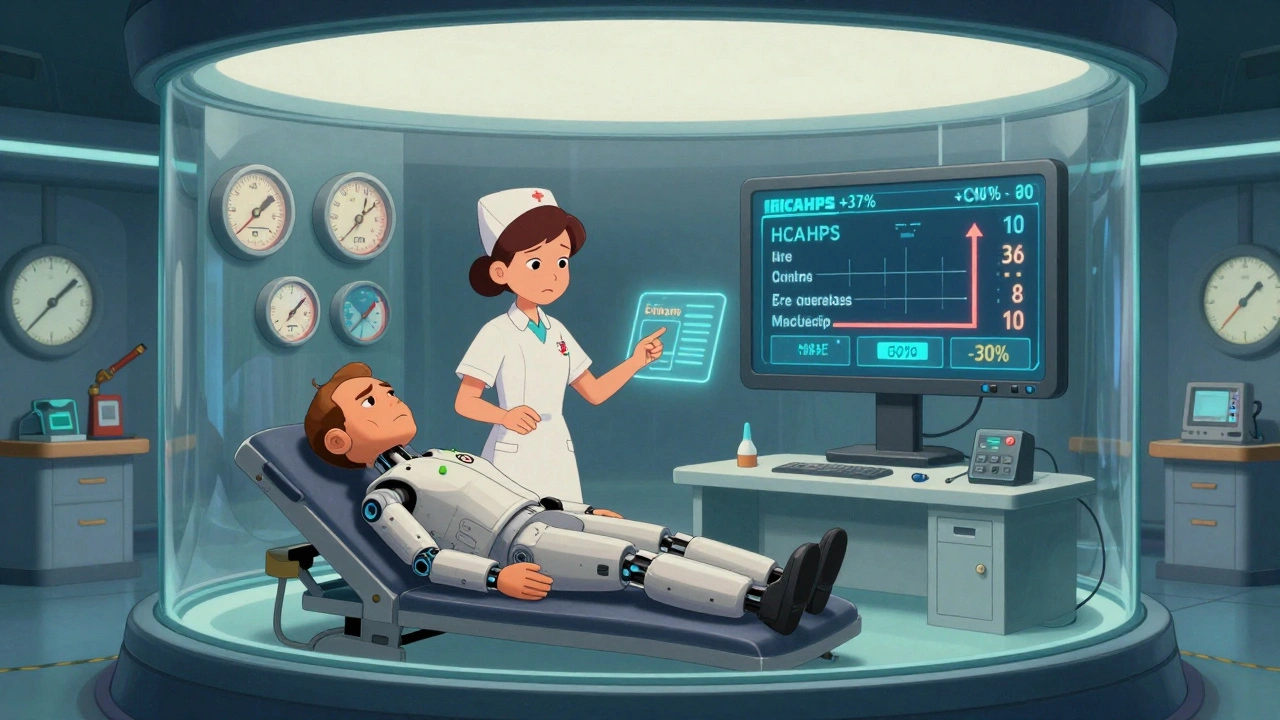
The Real Barriers to Success
Even the best programs fail if they’re not implemented right. The biggest problem? Time. Physicians average just 13.3 seconds before interrupting patients-even after training. A 2023 AAMC survey found 58% of clinicians said they knew the skills but didn’t have time to use them in 15-minute appointments. Another issue? Resistance. About 15-20% of staff see communication training as "fluffy" or "not for me." Mayo Clinic tackles this by having senior doctors lead sessions. When a respected attending physician says, "This changed how I talk to my patients," others listen. Faculty development is another bottleneck. Northwestern’s Dr. Vineet Arora found that without trained instructors who can give feedback, mastery learning doesn’t stick. That’s why successful programs spend 6-8 weeks preparing teachers before rolling out training to clinicians. And then there’s equity. A 2023 AHRQ report found a 28% communication satisfaction gap between white patients and minority patients. Most programs still don’t address cultural humility, implicit bias, or language barriers. But that’s changing. In January 2024, UT Austin launched three new HCTS modules focused specifically on communicating with diverse populations.How to Make It Work in Your Facility
If you’re trying to launch or improve a communication program, here’s what works:- Start with data. Look at your patient surveys. What complaints keep coming up? "Didn’t understand my meds"? "Felt rushed"? That’s your starting point.
- Focus on 3-5 behaviors. Don’t try to fix everything. Pick the top issues. For example: asking open-ended questions, checking for understanding, and summarizing next steps.
- Use real scenarios. Training with actors or video simulations beats PowerPoint every time. People remember stories, not slides.
- Embed it in workflow. Add prompts to your EHR. A pop-up that says, "Did you ask what matters most to the patient today?" makes the training stick.
- Find champions. Identify one or two respected staff members in each unit to model the behavior. Peer influence is 3x more powerful than top-down mandates.

What’s Next for Healthcare Communication
The field is evolving fast. AI is now being used to analyze patient-clinician conversations and give real-time feedback on tone, empathy, and clarity. Pilot programs show 22% faster skill acquisition with these tools. Telehealth is another big driver. With more visits happening over video, programs now include training on how to build rapport through a screen-reading micro-expressions, managing tech glitches, and ensuring patients feel seen even when they’re not in the room. The National Academy of Medicine just recommended that all clinicians be required to complete communication training. If that becomes policy, it could be the biggest shift in medical education since handwashing became standard. But sustainability remains a problem. Only 42% of hospital programs have dedicated funding. Many rely on grants or one-time training budgets. Without ongoing reinforcement, skills fade after six months. Tulane’s 2022 study showed that without regular practice, communication proficiency drops to 70% of peak levels.Final Thought: Communication Is a Skill, Not a Personality Trait
You can’t assume someone is a "good communicator" because they’re friendly. You can’t assume someone is "bad" because they’re quiet. Communication is a set of learnable skills-like suturing or interpreting an X-ray. And just like those skills, they need practice, feedback, and time to master. The institutions that invest in this-not as a compliance checkbox, but as a core part of patient care-are seeing fewer errors, higher satisfaction, and lower turnover. The data is clear. The tools exist. The question isn’t whether you should do it. It’s how soon you’ll start.Are healthcare communication programs only for doctors?
No. These programs are designed for everyone in the healthcare system-nurses, pharmacists, receptionists, social workers, and even administrators. Communication breakdowns happen at every level. A nurse who doesn’t clearly hand off a patient’s medication list, or a front desk staff member who doesn’t explain next steps, can cause serious errors. Programs like those from Mayo Clinic and SHEA train staff across roles with tailored content.
How long does it take to see results from communication training?
Initial improvements in patient satisfaction and staff confidence can show up in as little as 30 days. But real behavioral change-where skills become automatic-takes 3 to 6 months. Northwestern’s data shows skill retention spikes after 4-6 simulation sessions and continues to improve with monthly reinforcement. Without follow-up, skills decline after six months.
Do these programs work in rural or underfunded hospitals?
Yes, but they need adaptation. Rural facilities often lack simulation labs or dedicated trainers. That’s why free, self-paced options like UT Austin’s HCTS are so valuable. They can be done on phones or tablets during breaks. The key is starting small-train one champion per unit, use real patient stories for examples, and embed prompts in existing workflows. Even simple changes, like asking patients to repeat back instructions, can make a big difference.
Is communication training just about being nice to patients?
No. Being "nice" isn’t enough. Effective communication is about precision: knowing when to pause, how to ask open-ended questions, how to recognize fear or confusion in a patient’s tone, and how to confirm understanding. It’s not about being warm-it’s about being clear, accurate, and responsive. A study from Johns Hopkins found that physicians trained in these skills had 30% fewer malpractice claims-not because they were friendlier, but because they reduced misunderstandings that led to harm.
Can AI replace human communication training?
Not replace-enhance. AI tools can analyze recordings of patient visits and give feedback on word choice, pacing, and empathy levels. Some systems flag when a clinician interrupts too soon or uses too much jargon. But AI can’t model empathy or navigate cultural nuances. Human instructors are still essential for role-playing, giving personalized feedback, and building trust. The best programs use AI as a coach, not a replacement.
Why do some healthcare workers resist communication training?
Many feel it’s "soft" or unnecessary, especially if they’ve been practicing for years. Others fear being judged or exposed as "bad" communicators. The most effective programs address this by showing data: "This is why your patients are leaving confused," or "This is how your team’s miscommunication caused a delay." Peer modeling helps too-when respected colleagues share how the training changed their practice, resistance drops. It’s not about blame-it’s about improvement.
olive ashley
December 6, 2025 AT 14:34Let me guess - this is just another corporate buzzword scheme to make hospitals look good while cutting nurse hours. I’ve seen this ‘training’ before. They give you a 20-minute video on ‘active listening’ and then schedule 12 patients an hour. The real problem? Profit over people. They don’t care if you communicate - they care if you hit the billing quota. This is theater with a clipboard.
And don’t get me started on ‘standardized patients.’ Actors pretending to be scared? Please. Real patients don’t wait for your perfect pause. They’re in pain, confused, and terrified - and your ‘evidence-based’ script won’t fix that.
Also - AI analyzing tone? Cool. Now it’ll tell you you’re ‘too empathetic’ and flag you for inefficiency. Next thing you know, they’ll automate the entire bedside conversation. Who needs humans when you’ve got a chatbot that checks all the boxes?
They’re not fixing communication. They’re just making it more surveilled.
Ibrahim Yakubu
December 6, 2025 AT 20:00Ohhhhh so now we’re blaming doctors for not being ‘nice’ while hospitals in Nigeria are running on candles and hope? You think a 3.5-credit course in Maryland fixes what happens when a nurse has to treat 50 patients with one stethoscope? This is rich. I’ve seen clinics where the only ‘communication training’ is yelling over the generator noise.
Meanwhile, you Americans act like you invented empathy. We don’t need a PowerPoint on ‘closing the loop’ - we need clean water, electricity, and meds that don’t expire in 3 months. Your ‘data’ is meaningless when your system is built on insurance loopholes and billionaire boardrooms.
Stop romanticizing your broken system. We’re not failing because we didn’t attend a workshop - we’re failing because we’re ignored.
And yes - I’ve seen a child die because a pill bottle had no label. No ‘empathy training’ could’ve saved that.
Brooke Evers
December 7, 2025 AT 08:37I work in a rural ER, and I’ve seen firsthand how this training changes lives - not because it’s perfect, but because it gives people tools when they’re drowning.
One of our nurses, Maria, used to rush through discharge instructions. After the 6-week program, she started asking patients: ‘What’s the one thing you’re most worried about?’ That one question changed everything. One elderly man told her he was scared he’d die alone at home - he hadn’t told anyone before. She connected him with home health services. He’s still alive two years later.
It’s not about being ‘nice.’ It’s about being present. The training doesn’t fix the system - but it gives us moments where we can still be human.
And yes, it’s hard. We’re understaffed. We’re tired. But when you see a patient nodding, eyes wet, saying ‘finally someone listened’ - you keep going. Even if it’s just one person.
They say skills fade after six months? I’ve seen them stick when we do monthly ‘story circles’ - where staff share one patient interaction that mattered. No slides. Just voices. That’s the real magic.
Don’t write this off as fluff. It’s the only thing keeping some of us from burning out. And maybe - just maybe - it’s keeping patients alive.
Nigel ntini
December 9, 2025 AT 07:59This is an exceptionally well-researched and articulate piece. The integration of empirical data - particularly the Press Ganey correlation and the 30% reduction in malpractice claims - is compelling and rigorously cited. The distinction between performative empathy and structured, skill-based communication is critical and often misunderstood.
I would add that the success of these programs hinges on institutional culture, not merely curriculum design. A hospital that rewards speed over clarity will undermine even the most sophisticated training. Leadership must model the behavior - not just mandate it.
The mention of AI as a coaching tool is particularly forward-thinking. While it cannot replace human nuance, real-time feedback on linguistic patterns (e.g., excessive jargon, interruption frequency) offers scalable, objective improvement metrics.
However, I urge caution regarding equity. The 28% satisfaction gap between white and minority patients is not merely a training deficit - it is a systemic failure of cultural competency. Training must evolve beyond ‘talking to patients’ to ‘listening to their world.’
Well done. This should be required reading for every healthcare administrator.
Priya Ranjan
December 11, 2025 AT 06:26Oh please. You think training nurses to say ‘what’s your biggest concern’ fixes everything? You’re ignoring the real issue: patients are stupid. They don’t understand basic biology. They Google symptoms and panic. They show up with 17 questions and expect answers in 8 minutes.
And now we’re supposed to spend 20 minutes listening to someone who thinks ‘cancer is caused by WiFi’? No. We need to stop coddling ignorance. Doctors are trained to diagnose - not to be therapists for the delusional.
Also - why are we spending millions on ‘simulation actors’ when we could be hiring more nurses? This is woke nonsense dressed up as science. The real solution? Stop letting everyone walk into a hospital and demand attention. Triage properly. Stop rewarding incompetence with empathy.
Stop pretending communication is the problem. The problem is people who refuse to take responsibility for their own health.
And don’t even get me started on ‘cultural humility.’ We’re not here to validate beliefs - we’re here to fix bodies.
Gwyneth Agnes
December 11, 2025 AT 10:05Training doesn’t fix broken systems. Just sayin’.
Ashish Vazirani
December 11, 2025 AT 10:28Ohhhhhhh! So now the American medical system is the gold standard?!!? You think your fancy ‘standardized patients’ and ‘mastery learning’ means anything when India has 1 doctor for every 1,457 people?!?! You think your 3.5-credit course matters when our nurses work 72-hour shifts with no water?!?!
You want to fix communication?!?! Fix our hospitals first! Fix our power! Fix our drugs! Fix our corruption! Then come talk to me about ‘closing the loop’!
And don’t even mention ‘AI feedback’ - our clinics don’t have Wi-Fi! We use pen and paper and prayer!
You Americans think your way is the only way. But we survive. We adapt. We don’t need your expensive simulations. We need your money. Your vaccines. Your oxygen tanks.
This isn’t about communication. It’s about inequality dressed up as a TED Talk.
And I’m not mad. I’m just… exhausted.
Mansi Bansal
December 13, 2025 AT 07:43While the institutional frameworks delineated herein are commendable in their structural ambition, one must interrogate the epistemological underpinnings of such initiatives with rigorous scholarly scrutiny. The conflation of patient satisfaction metrics with clinical efficacy constitutes a profound methodological fallacy - a classic case of conflating phenomenological perception with ontological truth.
Moreover, the reliance on standardized actors as pedagogical proxies for authentic patient suffering introduces an artificiality that undermines the very integrity of clinical authenticity. Can one truly replicate the visceral terror of a terminal diagnosis through scripted scenarios? I submit: no.
Furthermore, the assertion that communication training reduces malpractice claims is statistically misleading; correlation does not imply causation. It is more plausible that such programs serve as risk-mitigation instruments designed to insulate institutions from litigation - not to enhance therapeutic outcomes.
One must also interrogate the neoliberal commodification of empathy: turning human connection into a measurable KPI, a performance metric, a box to be ticked on a hospital’s quarterly dashboard. This is not healing - it is administrative theater.
True healing arises from presence, not protocol. From silence, not scripts. From the unquantifiable, not the quantified.
Thus, while the architecture of these programs may appear robust, their philosophical foundation is brittle - and perilously close to the commodification of the sacred.
Max Manoles
December 13, 2025 AT 18:43I’ve been on both sides - as a nurse and now as a patient. My mom had a stroke, and the difference between the hospital that trained their staff and the one that didn’t? Night and day.
At the first hospital, they asked her what mattered most. She said, ‘I just want to see my grandkids.’ So they moved her bed to the window so she could see the playground. No one asked for permission. No one said ‘that’s not protocol.’ They just… did it.
At the other hospital? They read off a checklist. Asked her the same 5 questions. Didn’t look up once.
Training isn’t about scripts. It’s about seeing people. And when you do that, everything else follows.
Also - the part about ‘champions’? That’s real. We had a quiet tech who started asking patients, ‘What’s one thing you’re proud of?’ It became a thing. People started leaving notes. One woman wrote: ‘He made me feel like I still mattered.’
That’s not in any curriculum. But it’s the most important thing there is.
Rashmi Gupta
December 14, 2025 AT 05:38So let me get this straight - we’re going to fix medical errors by teaching doctors to ask better questions? Meanwhile, the FDA approves new drugs with zero long-term studies, insurance companies deny life-saving treatments, and hospitals hire CEOs who make $15 million while nurses get $22/hour.
Communication training is a distraction. A Band-Aid on a hemorrhage.
And yet you call this ‘evidence-based’? Funny - the same people pushing this are the ones who cut mental health services, defunded public clinics, and turned ERs into profit centers.
Fix the system. Not the words.
Andrew Frazier
December 15, 2025 AT 18:22Y’all act like this is some revolutionary breakthrough. We’ve been doing this in the military for decades. You don’t need a 3.5-credit course - you need discipline. You need structure. You need someone to yell at you when you screw up.
And don’t get me started on ‘cultural humility.’ We don’t need to ‘validate’ someone’s belief that aliens gave them cancer. We need to treat the tumor.
Also - AI feedback? Cool. But my grandma doesn’t need an algorithm telling her she’s ‘too abrupt.’ She needs someone who knows what they’re doing.
Stop treating medicine like a therapy session. It’s a science. Not a feel-good workshop.
Kumar Shubhranshu
December 17, 2025 AT 16:54Real talk: I work in a small clinic. We don’t have actors or AI. We have one laptop and 3 broken chairs.
But we do this: before every visit, we ask the nurse to say one thing they’re grateful for about the patient. Just one.
It changes everything.
Not because it’s fancy. Because it reminds us we’re not machines.
Simple. Free. Works.
Karen Mitchell
December 19, 2025 AT 13:08Another feel-good fantasy designed to make administrators feel virtuous while ignoring the real crisis: underfunding, understaffing, and profit-driven care.
Training won’t fix a system that pays doctors to see more patients, not to help them.
This isn’t progress. It’s performance.
And you’re all just dancing to the tune of the insurance companies.
Geraldine Trainer-Cooper
December 19, 2025 AT 20:02What if communication isn’t the problem? What if the problem is that we’ve turned healing into a transaction?
We don’t need more training. We need less hurry.
More silence.
More space for grief.
More time to just be with someone - not fix them.
Everything else is just noise.
Nava Jothy
December 20, 2025 AT 14:09Oh my GOD - this is so important!! 😭 I’ve been waiting for someone to say this!!
My aunt died because the nurse didn’t ask if she was scared. Just rushed through meds. No eye contact. No warmth. Just… efficiency.
And now you’re saying we can fix this?!?! With ACTORS?!?! With AI?!?!
It’s not enough. It’s never enough. But I’m crying right now because someone finally sees it.
PLEASE - can we make this mandatory? EVERYWHERE? I’ll start a petition!! I’ll fund it!! I’ll beg hospitals!!
My heart is breaking - but also… HOPEFUL??
Thank you. Thank you. Thank you. 💖
Brooke Evers
December 21, 2025 AT 15:24Max - your story about your mom? That’s the exact reason we started our ‘one thing you’re grateful for’ ritual. We didn’t call it anything fancy. Just a quiet moment before the door opened.
And Gwyneth - you’re right. Training doesn’t fix broken systems. But sometimes… it’s the only thing that lets us breathe long enough to keep fighting for the ones that do.
Thanks for saying that.