GLP-1 GI Side Effects: Meal Planning and Dose Titration Tips That Work
 Nov, 21 2025
Nov, 21 2025
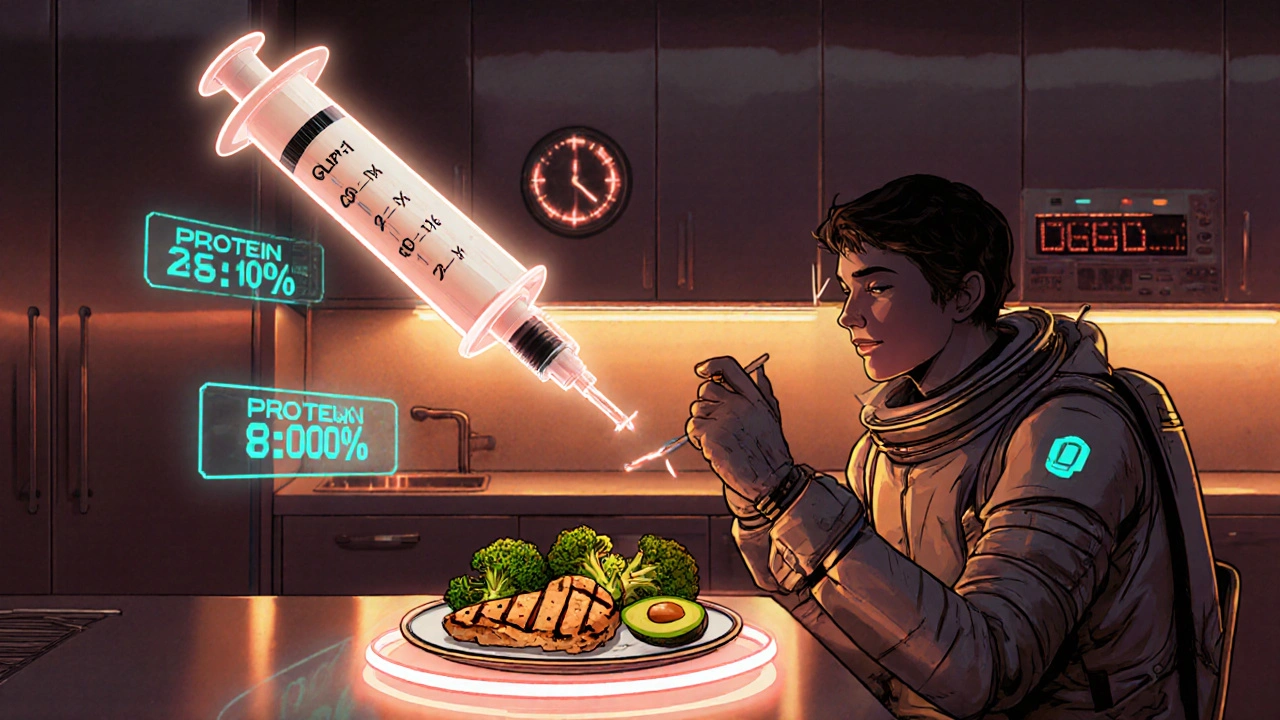
GLP-1 Meal Planner Calculator
Nutrient Guidelines
For optimal GLP-1 side effect management, aim for:
30g protein, under 40g carbohydrates, under 30g fat
Example Meal: 4oz grilled chicken, 1 cup steamed broccoli, 1/2 avocado
Enter values to see if your meal meets the guidelines
Why GLP-1 medications cause stomach problems-and how to fix them
GLP-1 receptor agonists like Ozempic, Wegovy, and Trulicity are changing how people manage type 2 diabetes and weight. But for nearly half of users, the benefits come with a price: nausea, vomiting, bloating, and diarrhea. These aren’t just mild annoyances-they’re the main reason people stop taking these drugs. The good news? Most of these side effects can be managed-or even avoided-with smart meal planning and a slow, patient approach to dosing.
How GLP-1 drugs mess with your digestion
These medications work by slowing down how fast your stomach empties. That’s great for controlling blood sugar and helping you feel full longer. But it also means food sits in your stomach longer, which triggers nausea and bloating. The brain’s vomiting center gets stimulated too, especially when you first start the drug. This isn’t a sign you’re doing something wrong-it’s a direct result of how the medicine works.
Studies show 40% to 70% of people on GLP-1 drugs experience GI side effects. Nausea hits hardest in the first few weeks, with up to 50% of users feeling sick. Vomiting affects 5% to 20%, and diarrhea shows up in 10% to 25%. The worst symptoms usually fade after 6 to 8 weeks-but only if you don’t push your body too hard too soon.
Why rushing your dose makes things worse
Pharmaceutical companies give you a standard titration schedule: increase your dose every week or two. But that’s designed for the average person. If you have a sensitive stomach, a history of IBS, or just don’t eat much protein, that schedule is a recipe for disaster.
Real-world data shows patients who stick to the fastest schedule are 2.5 times more likely to quit than those who go slower. The American Association of Clinical Endocrinology says extending titration to 20-24 weeks (instead of 16) cuts discontinuation by 35%. That’s not a suggestion-it’s a proven strategy.
Here’s what works: Don’t move up to the next dose until your nausea has been gone for at least 7 straight days. If you vomit more than twice in a week, hold your dose for 4-6 weeks. Some people need to stay at a lower dose for months. That’s not failure-it’s smart management.
The meal plan that reduces nausea by 40%
What you eat matters more than when you take the pill. Most people try to eat their usual meals-big portions, carbs, fried food-and wonder why they feel awful. The fix? A simple, consistent approach to food.
Registered dietitians at Joslin Diabetes Center recommend a 30-40-30 rule per meal during titration:
- 30 grams of protein
- Under 40 grams of carbohydrates (mostly fiber-rich, not sugar)
- Under 30 grams of fat
That means a meal like grilled chicken (4 oz), steamed broccoli (1 cup), and half an avocado hits the mark. A sandwich with white bread, mayo, and deli meat? Not even close.
People on Reddit’s r/Ozempic community who followed this pattern reported nausea dropping from daily to once a week. One user said: “I started eating 25g protein right after waking up. Within 3 days, I stopped feeling sick in the morning.”

Timing matters: When to eat, drink, and take your shot
It’s not just what you eat-it’s when.
- Take your weekly injection first thing in the morning, with just water.
- Wait 30 to 60 minutes before eating your first meal.
- Space meals 3 to 4 hours apart. No snacking between.
- Avoid eating within 3 hours of bedtime.
- Limit fluids to 4-6 oz (120-180 ml) with meals. Drink the rest between meals.
- Avoid soda, sparkling water, and alcohol completely during the first 8 weeks.
One Mayo Clinic patient shared that eating 2 hours after her injection reduced her nausea from severe to mild in just 3 days. That’s not magic-it’s pharmacology. When your stomach is empty, the drug has less to work against.
What to eat when nausea hits
If you’re feeling sick, don’t force yourself to eat a full meal. Go back to basics.
For the first 24-48 hours, stick to clear liquids: water, broth, herbal tea, or electrolyte drinks. Then move to the BRAT diet-bananas, rice, applesauce, toast. These are low-fiber, low-fat, and easy to digest.
Once you’re stable, slowly add back protein: boiled eggs, plain chicken, Greek yogurt, cottage cheese. Avoid dairy if it triggers bloating. Keep portions small: 300-400 calories per meal max. A 600-calorie meal during titration is a common reason people quit.
What not to do
Here are the top mistakes patients make:
- Trying to eat “normally” while on GLP-1 drugs
- Increasing the dose too fast because they “feel fine”
- Drinking large amounts of water with meals
- Skipping meals to avoid nausea (this makes it worse)
- Using anti-nausea meds without talking to their doctor
Skipping meals sounds logical, but it backfires. Your stomach needs gentle stimulation to adapt. Eating small, regular meals teaches your body to handle the slower emptying. Fasting or eating once a day can cause rebound nausea and even worsen gastroparesis.
When to call your doctor
Most GI side effects are temporary and manageable. But some signs mean you need help:
- Vomiting more than twice a week
- Unable to keep fluids down for 24 hours
- Severe abdominal pain or bloating that doesn’t improve
- Unexplained weight loss beyond your goal
- Dark urine, dizziness, or rapid heartbeat (signs of dehydration)
These could point to gastroparesis, bowel obstruction, or pancreatitis-rare, but serious. The FDA updated warnings for all GLP-1 drugs in January 2024 to highlight these risks. If you have any of these symptoms, pause your medication and talk to your provider.
What’s new in GLP-1 support
Drugmakers are finally catching on. Novo Nordisk now offers free dietitian consultations with Wegovy. Eli Lilly’s Mounjaro includes biweekly nurse check-ins during titration. Both report 15-20% higher adherence rates.
Major hospitals like Mayo Clinic and Cleveland Clinic now give patients “GLP-1 Starter Kits”-printed guides with meal plans, symptom trackers, and fluid schedules. One study showed ER visits for dehydration dropped 32% after these kits were introduced.
And soon, AI may help. Verily Life Sciences is testing an app that adjusts your dose schedule based on your daily symptom logs. Early results show a 28% drop in discontinuations.
Bottom line: Patience beats speed
GLP-1 drugs work. They lower A1C, reduce heart risk, and help you lose weight. But they’re not a quick fix. The people who succeed aren’t the ones who rush-they’re the ones who listen to their body.
Slow titration. Small meals. Protein first. No carbonation. Wait 60 minutes to eat. These aren’t just tips-they’re science-backed rules that keep people on the medication long-term.
If you’re struggling, you’re not alone. And you’re not failing. You’re just on the wrong schedule. Reset it. Slow down. Your stomach will thank you-and so will your health.
Henrik Stacke
November 22, 2025 AT 19:32Also, never drink soda with it. Sparkling water is a trap. Stick to still water between meals.
Manjistha Roy
November 24, 2025 AT 01:49Jennifer Skolney
November 24, 2025 AT 09:14JD Mette
November 25, 2025 AT 02:21Olanrewaju Jeph
November 26, 2025 AT 22:09Dalton Adams
November 28, 2025 AT 17:20Demi-Louise Brown
November 29, 2025 AT 01:42Matthew Mahar
November 30, 2025 AT 01:02