Generic vs. Brand Name Drugs: What You Need to Know About Bioequivalence and Cost Savings
 Jan, 27 2026
Jan, 27 2026
When you pick up a prescription, you might see two options: the familiar brand-name pill or a much cheaper generic version. You’ve probably wondered - is the generic just as good? Does it work the same? Or are you risking your health to save a few dollars? The truth is simpler than the fear suggests: generic drugs are not cheaper because they’re weaker. They’re cheaper because they don’t need to pay for ads, fancy packaging, or decades of research.
What Makes a Generic Drug a Generic Drug?
A generic drug isn’t a copy. It’s a legal, FDA-approved duplicate of a brand-name drug. To get approved, it must have the same active ingredient, strength, dosage form (tablet, capsule, liquid), and route of administration (swallowed, injected, etc.) as the original. That means if your brand-name drug is 10 mg of atorvastatin taken by mouth once daily, the generic must be exactly that - no more, no less. The key difference? The inactive ingredients. These are the fillers, dyes, or coatings that help the pill hold its shape or taste better. They don’t affect how the drug works. But here’s where confusion starts. Some people think their body reacts differently to these fillers. That’s rare - and usually not because the generic is bad. It’s because your body is sensitive to something new, even if it’s harmless.How Do We Know Generics Work the Same?
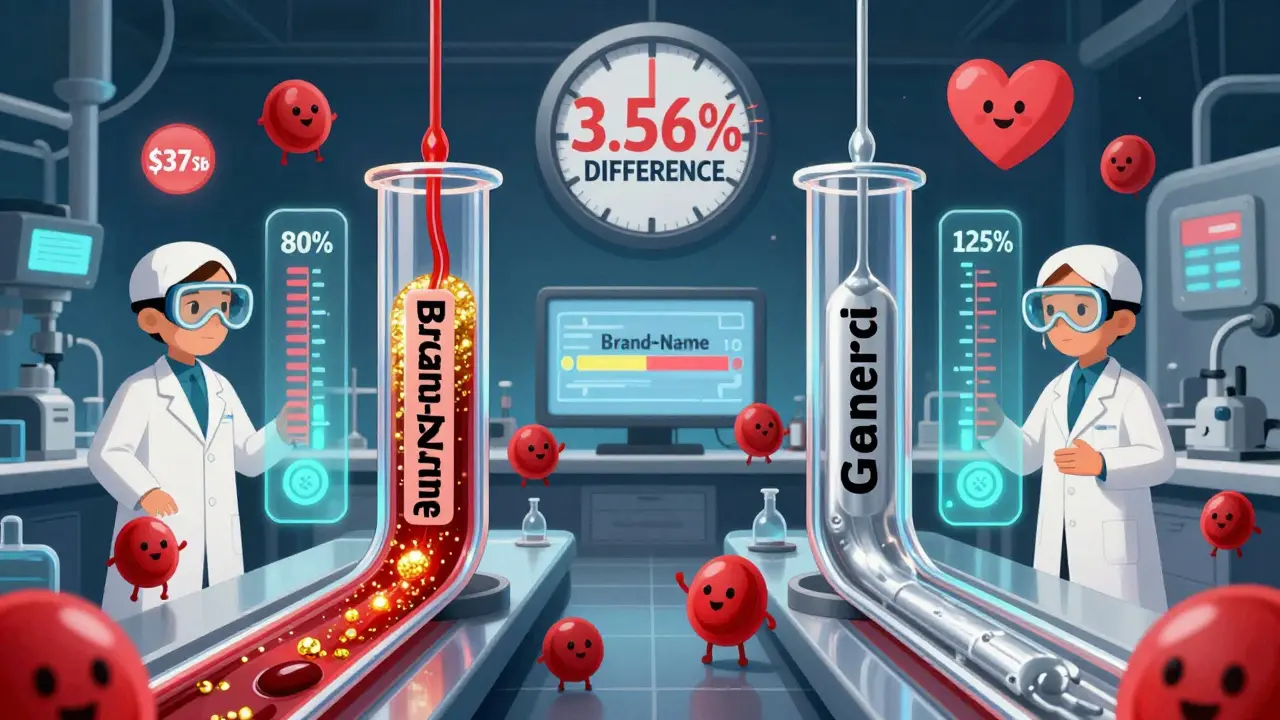
The FDA doesn’t just take a company’s word for it. Every generic must prove it’s bioequivalent to the brand-name version. That means it gets absorbed into your bloodstream at nearly the same rate and amount. Here’s how they test it: 24 to 36 healthy volunteers take both the brand and generic versions in a controlled study. Scientists measure two things: how high the drug peaks in your blood (Cmax) and how much total drug your body absorbs over time (AUC). For the generic to pass, these numbers must fall within 80% to 125% of the brand’s values. That’s not a wide gap - it’s tighter than the natural variation your body shows from day to day. Studies from 1996 to 2007 looked at over 2,000 of these tests. On average, the difference in absorption was just 3.56% for total exposure (AUC). That’s less than the fluctuation you get from eating a big meal before taking your pill. And 98% of those studies showed differences under 10%. The FDA calls this “clinically acceptable.” In plain terms: if you switch from brand to generic, your body won’t notice.Do Generics Really Save Money?
Yes. And not just a little. On average, generic drugs cost 80% to 85% less than their brand-name counterparts. That’s not marketing. That’s fact. In 2023, the U.S. healthcare system saved $373 billion because people chose generics instead of brands. That’s more than the entire GDP of Austria. Take Lipitor (atorvastatin). The brand cost around $335 for a 30-day supply. The generic? $0.00 with a GoodRx coupon. Plavix (clopidogrel)? Brand: $450. Generic: $0.00. You’re not getting a discount. You’re getting the exact same medicine at a fraction of the price. And it’s not just for rich people. Medicare Part D fills 92% of its prescriptions with generics. Commercial insurers? 87%. Generics aren’t a last resort - they’re the default because they work and they’re affordable.Are There Exceptions?
Yes. But they’re rare. Some drugs have a narrow therapeutic index (NTI). That means even tiny changes in blood levels can cause big problems - either the drug stops working or you get serious side effects. For these, doctors and pharmacists are extra careful. Examples include:- Warfarin (blood thinner)
- Levothyroxine (thyroid hormone)
- Phenytoin (seizure medicine)
- Lithium (mood stabilizer)
What About Patient Stories?
You’ve probably heard someone say, “I switched to generic and felt awful.” Or, “My grandma did fine on brand, but the generic made her dizzy.” These stories are real - but they’re not proof that generics are unsafe. They’re proof that people notice changes. When you switch from one pill to another, even if they’re chemically identical, the size, shape, color, or coating might be different. Your brain might associate the new look with “something’s wrong.” That’s psychological. It’s not the drug. A 2022 survey of 1,247 patients found 43% believed generics were less effective. But when researchers looked at actual outcomes, 89% of users reported no difference in how the drug worked. One big exception? Warfarin. A 2022 study found 61% of patients on warfarin refused to switch to generic - even though studies show no difference in safety or effectiveness. That’s fear, not fact.What About the Orange Book?
The FDA keeps a public list called the Orange Book. It’s the official record of which generics are rated as bioequivalent to brand-name drugs. Generics marked with an “AB” rating are interchangeable. That’s the gold standard. Pharmacists use this book every day. If a generic isn’t AB-rated, they won’t substitute it without asking your doctor. You can ask your pharmacist to check the Orange Book for you. They’re trained to do it.Why Do Brands Still Exist?
Because they’re profitable. Brand-name companies spend billions on marketing. They pay doctors to speak at events. They run ads on TV. They make you think their pill is better. But here’s the twist: a landmark 2020 study in Scientific Reports followed 1.2 million patients on 17 different drugs. It found that in 10 out of 17 cases, patients on generics had fewer deaths and heart attacks than those on brand-name versions. Why? Possibly because generics were cheaper, so people took them consistently. The brand-name users skipped doses because they couldn’t afford them. The real danger isn’t the generic. It’s not taking your medicine at all.
Phil Davis
January 29, 2026 AT 02:50So let me get this straight - we’re paying $300 for a pill that’s chemically identical to one that costs $0.05, and the only difference is the logo on it? Brilliant. Capitalism at its finest.
Katie Mccreary
January 30, 2026 AT 03:24My cousin took generic levothyroxine and started hallucinating. Yeah, sure, it’s ‘bioequivalent.’ Until your thyroid crashes and you’re sobbing in a Walmart parking lot at 3 a.m. You think science fixes that? Nah. It just gives you a PDF.
Jeffrey Carroll
January 31, 2026 AT 08:47The data presented here is compelling and aligns with decades of clinical evidence. Generic medications are subject to rigorous regulatory standards, and their efficacy is consistently validated through bioequivalence testing. The cost savings are not merely anecdotal but statistically significant and widely documented in peer-reviewed literature. For patients with chronic conditions, the financial accessibility provided by generics can be the difference between adherence and deterioration.
Lexi Karuzis
January 31, 2026 AT 21:36Wait… the FDA approves these? Who’s really running this? Big Pharma owns the FDA, right? And the Orange Book? That’s just a placebo for the masses. I read on a forum that generics have nano-scale contaminants from Chinese factories - they don’t even test for that. My aunt’s heart started racing after switching. They buried the study. They always bury the study.
Amber Daugs
February 2, 2026 AT 04:08People who take generics are just lazy. If you can’t afford the brand, maybe you shouldn’t be taking the drug at all. I mean, really - would you use a knockoff Rolex? No. So why would you risk your life on a knockoff heart pill? It’s not about money - it’s about responsibility.
matthew martin
February 3, 2026 AT 06:04Generics are the unsung heroes of modern medicine. You don’t hear them on TV, they don’t have TikTok influencers, and their packaging looks like it was designed by someone’s uncle who works at Staples. But they’re the reason I’m still here at 62, taking my blood pressure med every damn day. No fancy logo. No celebrity endorsement. Just science, savings, and sanity. Hats off to the pharmacists who quietly make this happen.
Chris Urdilas
February 3, 2026 AT 15:3985% cheaper? That’s not a discount - that’s a heist. The brand-name companies are basically charging you for the right to believe you’re getting something better. Meanwhile, the pill in your hand? Same molecule. Same effect. Same chance of not dying. Just without the $300 price tag and the jingle in your head. You’re not being smart by paying more. You’re being marketed to.
SRI GUNTORO
February 5, 2026 AT 03:22In my country, we don’t have this problem. We trust our doctors, not corporations. Why do Americans need to be convinced that medicine is medicine? It’s like arguing whether water is wet. You people overthink everything.
Mindee Coulter
February 6, 2026 AT 10:44I switched to generic Lipitor last year. No difference. Still alive. Still got my cholesterol under control. Also saved $280/month. Win-win.
Rhiannon Bosse
February 7, 2026 AT 10:49Okay but what if the generic is made in a factory that also makes rat poison? I saw a video. The guy had a lab coat and a clipboard. He said the dye in the generic Plavix was the same as in the new iPhone 15 screen. And that’s not even the creepiest part. The coating? It’s the same as what’s used in some weight loss teas. I’m not taking it. I’d rather die rich.
Mark Alan
February 8, 2026 AT 07:07USA > EVERYONE. We invented medicine. We invented patents. We invented the right to pay $400 for a pill that should cost $1. If you can’t afford it, move to India. Or better yet - don’t get sick. That’s the American way.
Linda O'neil
February 8, 2026 AT 19:23As a pharmacist for 22 years, I’ve seen it all. Patients panic when they get a different-colored pill. I show them the Orange Book. I explain the 80–125% bioequivalence window. I tell them the difference between generics is smaller than the difference between their morning and evening blood pressure. Most of them just need to hear it from someone they trust. It’s not about the drug - it’s about fear. And we can fix that.
Kevin Kennett
February 10, 2026 AT 00:40I used to be one of those people who’d only take brand-name. Then I got laid off. Switched to generic metformin. Didn’t die. Didn’t get dizzy. Didn’t turn into a zombie. My A1c stayed the same. My wallet? Thank you. If you’re scared, talk to your pharmacist. They’re not trying to kill you. They’re trying to keep you alive without you going broke.
Howard Esakov
February 10, 2026 AT 07:58Let’s be clear - generics are for the plebs. The elite don’t take them. We know the difference. We pay for the consistency, the brand trust, the psychological reassurance. You think a CEO takes a generic beta-blocker? No. He takes the one with the embossed logo. Because when you’re running a Fortune 500 company, you don’t gamble with your physiology. You invest in certainty. And yes - that certainty costs money. That’s not greed. That’s wisdom.
Robert Cardoso
February 11, 2026 AT 15:17Here’s the philosophical problem: if two substances are bioequivalent, are they truly identical? Or are they just functionally equivalent? The molecule is the same, sure - but the context isn’t. The placebo effect isn’t a bug, it’s a feature. The brand-name pill carries the weight of cultural trust, of medical authority, of decades of advertising that shaped your nervous system’s expectation of efficacy. To dismiss that as ‘just psychology’ is to misunderstand the biology of belief. Your body doesn’t just absorb molecules - it absorbs meaning. And meaning has pharmacokinetics.