Diabetic Retinopathy Screening Intervals and Treatment Options: What You Need to Know in 2026
 Jan, 11 2026
Jan, 11 2026
Diabetic retinopathy isn’t just a complication of diabetes-it’s the leading cause of preventable blindness in adults under 65. And yet, nearly one in three people with diabetes don’t get the eye exams they need. Many think if their vision feels fine, they’re safe. That’s a dangerous myth. By the time blurry vision shows up, damage is often already advanced. The good news? With the right screening schedule and timely treatment, up to 98% of severe vision loss from diabetic retinopathy can be prevented.
How Diabetic Retinopathy Progresses
Diabetic retinopathy happens when high blood sugar damages the tiny blood vessels in the retina-the light-sensitive layer at the back of your eye. At first, these vessels leak fluid or bleed slightly. That’s called nonproliferative diabetic retinopathy (NPDR). Most people with diabetes have this early stage, and it often causes no symptoms. But if it worsens, new, fragile blood vessels start growing on the retina’s surface. That’s proliferative diabetic retinopathy (PDR). These vessels are weak. They bleed easily, cause scar tissue, and can pull the retina away from the back of the eye-leading to sudden, permanent vision loss.Diabetic macular edema (DME) is another major risk. It’s when fluid builds up in the macula, the part of the retina responsible for sharp, central vision. Even if retinopathy is mild, DME can still develop and blur your ability to read, drive, or recognize faces. About 7% of people with diabetes develop DME at some point.
The progression isn’t the same for everyone. Someone with well-controlled blood sugar and normal blood pressure might have stable mild NPDR for years. Another person with HbA1c above 9%, high blood pressure, and kidney problems could go from no retinopathy to sight-threatening disease in less than a year.
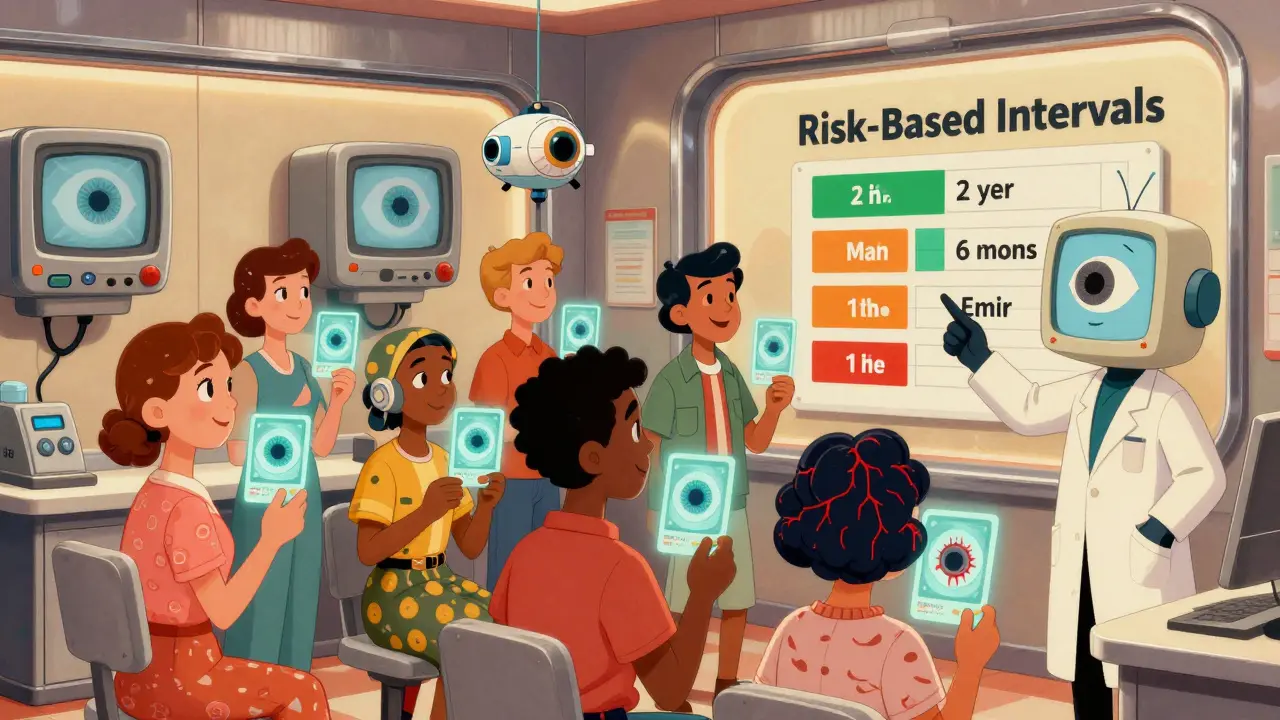
When to Get Screened: Risk-Based Intervals
Gone are the days when everyone with diabetes got an eye exam every year, no matter what. Today, screening is personalized. The goal isn’t just to check your eyes-it’s to catch sight-threatening changes early, without overburdening low-risk patients.Here’s what current guidelines say based on your risk level:
- No retinopathy or mild NPDR: Screen every 1-2 years. If you’ve had two or more clean screenings and your HbA1c is under 7%, blood pressure is controlled, and you have no kidney damage, extending to every 2 years is safe. For type 2 diabetes patients with no retinopathy at diagnosis, some experts now recommend screening every 3-4 years if risk factors are low.
- Moderate NPDR: See an ophthalmologist within 3-6 months. This stage means the disease is progressing. You’re not in immediate danger, but you need closer monitoring.
- Severe NPDR: Must be evaluated within 3 months. The risk of turning into proliferative retinopathy jumps significantly. Delaying care increases the chance of irreversible damage.
- Proliferative DR or DME: See a specialist within 1 month. These are emergencies. Waiting even 6 weeks can cost you vision.
For type 1 diabetes, screening starts 3-5 years after diagnosis. For type 2, it begins at diagnosis because many people have had undiagnosed high blood sugar for years before being diagnosed with diabetes.
Tools like RetinaRisk help doctors calculate your personal risk using your HbA1c, diabetes duration, blood pressure, and kidney function. One 2023 study found that using this model reduced unnecessary screenings by 59% without missing a single case of sight-threatening disease.
What Happens During a Screening
A diabetic eye screening isn’t just a quick glance. It’s a detailed imaging process. Most clinics now use digital fundus photography-taking high-resolution pictures of your retina after dilating your pupils. Two images per eye are standard: one focused on the macula and one on the optic nerve. This gives a full view of the retina’s condition.Some clinics use AI-powered tools like IDx-DR or Google Health’s DeepMind algorithm. These systems analyze the images and flag cases needing urgent attention. In a 2022 JAMA study, DeepMind detected referable retinopathy with 94.5% accuracy-matching or exceeding human graders.
For patients in rural areas or those with limited access to specialists, telemedicine screening is growing fast. A 2022 study called IDEAS showed that remote screening had 94% sensitivity for spotting serious retinopathy. A nurse or technician takes the photos, and a specialist reviews them later. It’s fast, affordable, and effective.
Treatment Options: From Laser to Injections
If your screening finds sight-threatening retinopathy or DME, treatment isn’t optional-it’s urgent. The good news? Modern treatments are highly effective.- Anti-VEGF injections: These are now the first-line treatment for DME and severe PDR. Drugs like ranibizumab (Lucentis), aflibercept (Eylea), and bevacizumab (Avastin) block a protein that causes abnormal blood vessels to grow. Injections are given directly into the eye, usually every 4-8 weeks at first. Most patients see improved vision or stop losing it. Some even regain lost vision.
- Laser therapy: Focal laser treats leaking blood vessels in DME. Panretinal photocoagulation (PRP) shrinks abnormal vessels in PDR. It’s not perfect-some patients lose peripheral or night vision-but it’s proven to prevent blindness in over 90% of cases.
- Steroid implants: For patients who don’t respond well to anti-VEGF drugs, tiny implants like Ozurdex release steroids slowly inside the eye. They reduce swelling but can raise eye pressure or cause cataracts, so they’re used carefully.
- Vitrectomy: If there’s a major bleed into the vitreous or retinal detachment, surgery may be needed. This involves removing the cloudy gel from the eye and repairing the retina.
Early treatment makes all the difference. One study found that patients treated within 1 month of developing PDR had 75% better vision outcomes than those who waited 3 months.
What You Can Do to Prevent Progression
Screening and treatment are critical-but they’re not the whole story. Your daily choices matter just as much.- Keep HbA1c under 7%: The DCCT/EDIC trials showed that intensive glucose control reduced retinopathy risk by 76% in type 1 diabetes and slowed progression by 54% in those already affected.
- Control blood pressure: Keeping systolic pressure below 140 mmHg reduces the risk of retinopathy progression by 34%. If you have kidney disease, aim for 130/80.
- Manage cholesterol: High LDL worsens retinal damage. Statins may help protect your eyes, even if your cholesterol is only mildly elevated.
- Don’t smoke: Smoking doubles your risk of developing diabetic retinopathy and speeds up its progression.
- Get regular exercise: Even 30 minutes of walking five days a week improves blood sugar control and circulation.
And don’t forget pregnancy. Women with diabetes who get pregnant are at high risk for rapid retinopathy progression. Eye exams are recommended in the first trimester and again in the third trimester, with follow-up one year after delivery.
Why Many People Miss Their Screenings
Despite the clear benefits, screening rates in the U.S. are only 58-65%. Why?Some people don’t realize diabetes affects the eyes. Others can’t afford the visit, especially if they lack insurance. Rural areas have fewer eye specialists. Some clinics still use outdated annual schedules, confusing patients who’ve been told they’re low-risk.
One Reddit user, ‘RetinaScared2023,’ shared how their clinic pushed for 2-year screenings despite an HbA1c of 8.5%. They developed macular edema within a year. Another, ‘Type1Warrior87,’ said switching to biennial exams after three clean screenings reduced their anxiety and saved them time and money.
The problem isn’t lack of knowledge-it’s inconsistent care. Not every provider uses risk-stratified guidelines. If your doctor hasn’t mentioned your individual risk level, ask. Don’t assume you’re low-risk just because you feel fine.
The Future: AI, Smart Devices, and Equity
The future of diabetic eye care is moving fast. AI tools are now FDA-cleared and integrated into primary care clinics. Devices like the D-Eye smartphone adapter let nurses or even patients themselves take retinal photos at home. These are game-changers for rural communities and people with mobility issues.But technology alone won’t fix everything. Low-income populations have 2.3 times higher rates of blindness from diabetic retinopathy-even though their diabetes rates are similar. The real challenge is access. Programs that bring screening to community centers, pharmacies, and mobile clinics are showing promise. The WHO estimates that if risk-stratified screening is scaled globally, 2.5 million cases of blindness could be prevented by 2030.
The message is clear: diabetic retinopathy doesn’t have to mean blindness. But you have to be proactive. Know your risk. Get screened on the right schedule. Treat it early. And don’t wait for symptoms.
How often should I get screened for diabetic retinopathy if I have type 2 diabetes and no eye problems?
If you have type 2 diabetes and no signs of retinopathy on your first exam, and your HbA1c is under 7%, blood pressure is controlled, and you have no kidney damage, you can safely wait 2-3 years before your next screening. After two consecutive clean exams, some guidelines allow extending to every 3-4 years. But if your HbA1c is above 8%, or you have high blood pressure or kidney disease, annual screening is still recommended.
Can diabetic retinopathy be reversed?
Early damage from diabetic retinopathy can sometimes improve with treatment. Anti-VEGF injections and laser therapy can reduce swelling and stop abnormal blood vessel growth, which may restore some lost vision-especially if treated early. However, once scar tissue forms or the retina detaches, the damage is permanent. That’s why early detection is so critical.
Are eye injections for diabetic retinopathy painful?
Most patients feel only mild discomfort. The eye is numbed with drops before the injection, and the needle is very thin. The whole process takes less than a minute. Some people feel pressure or a brief stinging sensation. Afterward, your eye may feel scratchy or red for a day or two, but serious pain is rare. The benefits far outweigh the temporary discomfort.
What if I don’t have insurance? Can I still get screened?
Yes. Many community health centers, nonprofit eye clinics, and mobile screening programs offer free or low-cost diabetic eye exams. The American Diabetes Association partners with local organizations to provide screenings in underserved areas. Some pharmacies and Walmart Vision Centers also offer basic retinal imaging for under $50. Don’t let cost stop you-early detection saves vision and saves money long-term.
Can I rely on my regular eye doctor instead of a specialist?
For screening, yes-many optometrists are trained to detect diabetic retinopathy using digital imaging. But if your screening shows moderate or worse retinopathy, you’ll need to see a retina specialist (ophthalmologist). They’re the only ones who can perform laser treatments, injections, or surgery. Your optometrist will refer you if needed. Regular eye exams for glasses or contacts aren’t enough-you need a diabetic-specific screening.
Does controlling my blood sugar stop diabetic retinopathy from getting worse?
Absolutely. The DCCT and EDIC studies proved that keeping HbA1c under 7% cuts the risk of developing retinopathy by 76% in type 1 diabetes and slows progression by over half in those who already have it. Even small improvements-like lowering HbA1c from 9% to 8%-make a measurable difference. Blood sugar control is the most powerful tool you have to protect your vision.
Prachi Chauhan
January 12, 2026 AT 17:13It's wild how we treat diabetes like it's just about insulin and pills, but the real silent killer is in your eyes. I never thought about my retina until my cousin lost vision. Now I get screened every year, even though my HbA1c is 6.8. Better safe than blind, right?
Also, why do doctors still push annual exams for everyone? If your numbers are good and you're not smoking, why not stretch it to two years? Saves time, money, and stress.
Katherine Carlock
January 14, 2026 AT 01:04I love that AI is finally helping with this! My dad got screened via a smartphone adapter at his local pharmacy last year - $35, no dilation, took 5 minutes. The results came back in 2 days and he got referred for a follow-up. No drama, no waiting 6 months for an appointment. Tech is saving lives, not just making TikToks 😊
Sona Chandra
January 14, 2026 AT 20:03THIS IS WHY PEOPLE ARE DYING. Your doctor says 'come back in 2 years' and you're like 'cool' and then BAM - you're legally blind and they say 'well you should've been screened more often.' NO. YOU SHOULD'VE BEEN WARNED. I had a friend who got told she was low risk - HbA1c 8.9, BP 150/95, kidney protein in urine - and they still said 'every two years.' She lost her vision in 11 months. THIS IS MALPRACTICE. Someone needs to sue these clinics.
Jennifer Phelps
January 14, 2026 AT 22:25So anti VEGF injections are the new standard but how much do they actually cost because I read somewhere that Eylea is like 2k per shot and you need like 6 a year and that's 12k just for the drug not counting the clinic fees and the travel and the time off work and also what if your insurance denies it because you're not 'severe enough' yet but you're already getting blurry and your doctor says wait until it's worse
also is it true that Avastin is cheaper but not FDA approved for eyes and some docs use it anyway and is that legal
beth cordell
January 15, 2026 AT 21:59Just got my screening today 🙌🏻 and guess what - no retinopathy! 🎉 HbA1c 6.4, BP 128/78, no kidney issues. I waited 3 years because my doc said I was low risk and I'm so glad I listened. Also got a free eye exam at Walmart Vision for $40 - total win 🥳
PS: If you're scared of injections, I did 3 last year and it felt like a tiny pinch. Like a mosquito but in your eyeball 😅
Lauren Warner
January 17, 2026 AT 10:59Let’s be real - this whole screening system is a scam designed to keep ophthalmologists rich. AI detects the disease with 94% accuracy but they still make you pay $200 for a 'specialist review.' Meanwhile, people in rural areas can't even get a phone to take a photo. And don’t get me started on the insurance hoops. You need a referral, a prior auth, a second referral, and then they say 'your condition isn't severe enough for coverage.' So you wait. And your retina dies. This isn't healthcare. It's a profit model disguised as prevention.
Jose Mecanico
January 19, 2026 AT 05:21I’ve been managing type 2 for 12 years and never had an issue until last year. My optometrist caught mild NPDR during a routine check. I was shocked because I felt fine. Now I get screened every 18 months, my HbA1c is 6.1, and I walk 45 minutes daily. It’s not hard - just consistent. Don’t wait for symptoms. Your eyes don’t scream before they break.
Alex Fortwengler
January 20, 2026 AT 10:15AI screening? Really? You think a machine can read your retina better than a real doctor? LOL. These companies are just pushing tech so they can replace humans and cut costs. And who’s gonna pay for it? The poor. Meanwhile, the real problem is Big Pharma pushing expensive injections so you stay hooked for life. Avastin works just fine and costs $50. Why are they hiding it? Because they don’t make billions off it. Wake up. This isn’t medicine - it’s corporate control.
jordan shiyangeni
January 22, 2026 AT 03:42It’s astonishing how many people still believe that if they ‘feel fine,’ they’re safe. This is not merely ignorance - it is a profound failure of public health education. The retina is not a muscle that responds to pain; it is a delicate neural tissue that deteriorates silently, often irreversibly. The DCCT trial, published in the New England Journal of Medicine in 1993, demonstrated unequivocally that intensive glycemic control reduces microvascular complications by 76 percent. Yet, here we are, three decades later, and patients are still being told to ‘wait and see.’ This is not negligence - it is systemic malfeasance. You are not being proactive if you wait for blurry vision. You are being a statistic. And if you are relying on your optometrist to detect proliferative retinopathy without dilation, you are gambling with your sight. There is no excuse. Not anymore.
Abner San Diego
January 22, 2026 AT 08:52Why are we even talking about this like it’s a medical mystery? It’s simple: if you’re diabetic and you’re not poor, you get screened. If you’re poor, you wait until you can’t see the TV. The system is rigged. We have the tech, the science, the AI - but we don’t have the will to make it free. Why? Because someone’s making money off your blindness. I’m not saying don’t get checked - I’m saying don’t trust the system. Fight for your rights. Demand community screenings. Don’t let them turn your eyes into a profit center.
Eileen Reilly
January 23, 2026 AT 02:44okay so i got my screening and they said i had mild npdr and i was like ok cool but then the doc said i need to see a specialist in 4 months and i was like wait i thought i was low risk?? my hba1c is 7.2 and i dont smoke but i do have high bp and my kidney thingy was kinda weird last year so maybe i shoulda listened to the reddit post from last week about how even if you feel fine you gotta go
also the lady at the clinic was super nice and used this new camera that looked like a space gun lol
Prachi Chauhan
January 23, 2026 AT 15:09Replying to Eileen - I had the same panic. Thought I was low risk, then got flagged for moderate NPDR. Turns out, 'mild' doesn't mean 'safe.' My doc didn't explain the progression clearly. Now I know: mild NPDR is a warning sign, not a green light. I started walking daily and cut out soda. My HbA1c dropped to 6.5 in 3 months. Don't wait for a specialist to scare you - start now.