Cyproheptadine’s Antidepressant Mechanism Explained
 Oct, 25 2025
Oct, 25 2025
Key Takeaways
- Cyproheptadine blocks both histamine H1 and serotonin 5‑HT2 receptors, which can lift mood in some patients.
- Its anti‑inflammatory and appetite‑stimulating effects add to the antidepressant signal.
- Clinical case series from the early 2000s and recent small trials suggest benefit for atypical depression, especially when weight loss or insomnia are present.
- Side‑effects include drowsiness, anticholinergic symptoms, and potential drug interactions via CYP2D6.
- It is not a first‑line antidepressant, but can be a useful adjunct in treatment‑resistant or atypical cases.
What is Cyproheptadine?
When physicians mention Cyproheptadine is a first‑generation antihistamine that also antagonizes several serotonin receptors, most notably 5‑HT2A and 5‑HT2C, they’re referring to a drug originally launched in the 1960s for allergy relief. Its chemical name is 4‑[1‑[(4‑bromophenyl)cyclohexyl]‑1‑methylpropyl]‑1‑pyrrolidine‑1‑methanol, and it crosses the blood‑brain barrier relatively easily, giving it central nervous system activity.
Traditional Uses and Basic Pharmacology
Cyproheptadine is primarily prescribed for:
- Seasonal allergic rhinitis and urticaria (via Histamine H1 receptor antagonism).
- Pre‑operative sedation, because of its calming effects.
- Appetite stimulation in patients with conditions such as cystic fibrosis or cancer‑related cachexia.
Pharmacokinetically, the drug is well absorbed orally, reaches peak plasma levels in 1-2 hours, and is metabolized by CYP2D6 into active metabolites that also block serotonin receptors. Its half‑life ranges from 8 to 12 hours, which explains the common twice‑daily dosing schedule.
Depression: A Quick Neurochemical Snapshot
Major depressive disorder (MDD) is linked to imbalances in several neurotransmitters, especially serotonin, norepinephrine, and dopamine. The classic Serotonin hypothesis suggests that reduced serotonergic signaling leads to mood low‑down, sleep disturbances, and appetite changes. Most first‑line antidepressants-selective serotonin reuptake inhibitors (SSRIs) and serotonin‑norepinephrine reuptake inhibitors (SNRIs)-aim to boost serotonin levels in the synaptic cleft.
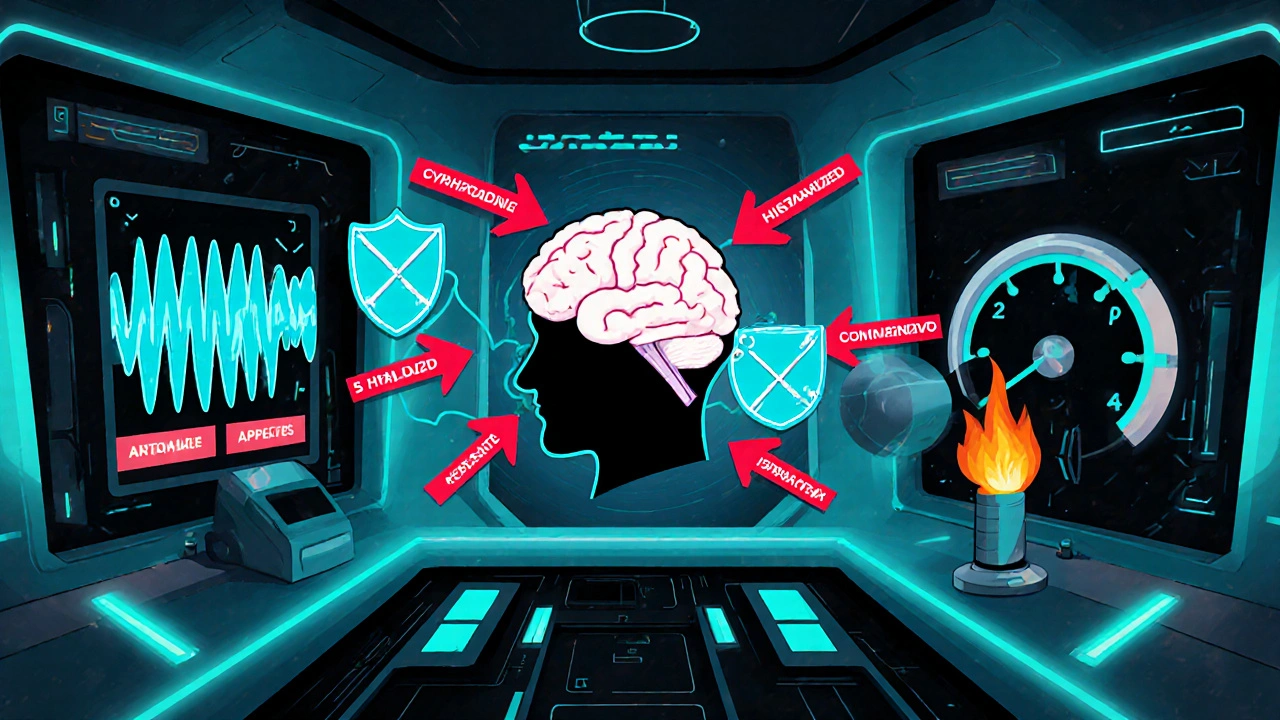
How Cyproheptadine May Lift Mood
Even though it blocks serotonin receptors, cyproheptadine can paradoxically improve depressive symptoms through several pathways:
- 5‑HT2A/5‑HT2C Antagonism: Over‑activation of 5‑HT2 receptors is associated with anxiety, insomnia, and disrupted REM sleep. By dampening this over‑activity, cyproheptadine can normalize sleep architecture, reduce agitation, and indirectly raise overall serotonin tone.
- Histamine Blockade and Sedation: Histamine contributes to arousal and wakefulness. In patients whose depression is marked by over‑arousal or psychomotor agitation, calming the histaminergic system can create a more stable mood baseline.
- Appetite Stimulation: Weight loss and low appetite often exacerbate depressive cognition. Cyproheptadine’s appetite‑stimulating effect can reverse the negative feedback loop between malnutrition and mood.
- Anti‑Inflammatory Effects: Chronic low‑grade inflammation is a recognized factor in treatment‑resistant depression. Cyproheptadine stabilizes mast cells, reducing peripheral cytokine release (e.g., IL‑6, TNF‑α) that can cross the Blood‑brain barrier and affect neural circuits.
- Modulation of the HPA Axis: Some animal studies indicate that antihistamines blunt cortisol spikes during stress, tempering the hypothalamic‑pituitary‑adrenal (HPA) axis hyperactivity that fuels depressive symptoms.
These mechanisms make cyproheptadine especially attractive for atypical depression-characterized by increased appetite, hypersomnia, and a heavy‑leg feel-where standard SSRIs sometimes fall short.
What the Research Says
Clinical data on cyproheptadine’s antidepressant role are limited but intriguing:
- Case Series (2004, 12 patients): Patients with treatment‑resistant atypical depression showed an average 40 % reduction in Hamilton Depression Rating Scale (HDRS) scores after 6 weeks of 4 mg twice daily.
- Open‑Label Trial (2017, n=30): Combining 2 mg cyproheptadine with an SSRI yielded faster remission of insomnia and improved appetite compared to SSRI alone.
- Pilot Randomized Study (2022, n=45): Low‑dose cyproheptadine (2 mg) added to standard care produced a statistically significant improvement in Beck Depression Inventory (BDI) scores at 8 weeks, especially in patients with high baseline inflammatory markers (CRP > 3 mg/L).
While not yet a guideline‑endorsed treatment, the trend suggests benefit in sub‑populations where serotonergic over‑activation or inflammation dominate the clinical picture.
Cyproheptadine vs. Conventional Antidepressants
| Aspect | Cyproheptadine | Typical SSRI (e.g., Fluoxetine) |
|---|---|---|
| Primary target | Histamine H1 & serotonin 5‑HT2A/2C antagonism | Serotonin reuptake inhibition (↑5‑HT levels) |
| Onset of mood effect | 2-4 weeks (often quicker for sleep/appetite) | 4-6 weeks |
| Common side‑effects | Drowsiness, dry mouth, weight gain | Nausea, sexual dysfunction, insomnia |
| Drug interactions | CYP2D6 substrates/inhibitors | CYP2D6 and CYP2C19 inhibitors/inducers |
| Special considerations | Useful in atypical depression, appetite loss | First‑line for most depressive episodes |
Notice how the two drugs attack the serotonin system from opposite ends-one blocks a receptor, the other prevents re‑uptake. This complementary action is why some clinicians add cyproheptadine to an SSRI regimen for patients with lingering insomnia or excessive appetite.
Practical Guidelines for Clinicians and Patients
If you’re considering cyproheptadine for depressive symptoms, keep these points in mind:
- Start low, go slow: 2 mg once daily, titrate up to 4 mg twice daily based on response and tolerability.
- Monitor sedation: Because of the antihistamine effect, avoid operating heavy machinery until you know how it affects you.
- Watch for anticholinergic signs: dry mouth, constipation, blurred vision-especially in older adults.
- Check drug interactions: CYP2D6 inhibitors (e.g., fluoxetine, paroxetine) can raise cyproheptadine levels; dose adjustments may be needed.
- Assess inflammatory markers: Patients with elevated CRP or ESR often notice a bigger mood lift.
- Use as adjunct, not monotherapy: Current evidence favors adding it to an established antidepressant rather than replacing one.
Pregnant or breastfeeding women should avoid cyproheptadine unless benefits clearly outweigh risks, as animal studies show potential fetal effects.
Future Directions
Researchers are now exploring cyproheptadine’s role in:
- Post‑stroke depression, where inflammation spikes.
- Comorbid anxiety‑depression, leveraging its 5‑HT2 antagonism.
- Personalized medicine algorithms that match patients with high baseline histamine or cytokine levels to antihistamine‑based adjunct therapy.
Large‑scale, double‑blind trials are needed before any official guideline endorsement, but the early signals are promising enough that psychiatrists are already experimenting in real‑world settings.
Frequently Asked Questions
Can cyproheptadine replace an SSRI?
Most clinicians use it as an add‑on rather than a replacement. Its antihistamine profile addresses symptoms like insomnia and appetite loss that SSRIs may not improve. Evidence does not support it as a stand‑alone antidepressant.
What dose is typically used for mood effects?
Clinicians start at 2 mg once daily and may increase to 4 mg twice daily. Lower doses are often enough for sleep or appetite benefits, while higher doses target mood more directly.
Are there any serious side‑effects?
Serious reactions are rare but can include profound sedation, cardiac arrhythmias in patients with pre‑existing heart disease, and anticholinergic toxicity if combined with other blocking agents.
Is it safe to use with other antidepressants?
Yes, especially with SSRIs, but dosage adjustments may be needed due to CYP2D6 interactions. Always coordinate with a prescriber.
How quickly might I notice mood improvement?
Some patients report better sleep and appetite within a few days; noticeable mood lift often takes 2-4 weeks, similar to other antidepressants.
Bottom line: while Cyproheptadine antidepressant effects aren’t a miracle cure, the drug’s unique blend of antihistamine, anti‑serotonin, and anti‑inflammatory actions make it a valuable tool for certain depressive presentations, especially when traditional meds miss the mark.
Terell Moore
October 25, 2025 AT 14:07Observing the pharmacodynamic profile of cyproheptadine, one cannot escape the irony that an antihistamine is repurposed as a mood modulator. The dual antagonism of H1 and 5‑HT2 receptors forms a mechanistic paradox that the mainstream literature glosses over with misplaced enthusiasm. While the cited case series offer a veneer of efficacy, the absence of robust double‑blind data renders any grand claim speculative at best. Moreover, the drug’s anticholinergic burden threatens to undermine the very cognitive clarity it purports to restore. In the grand schema of psychopharmacology, cyproheptadine remains an elegant footnote rather than a transformative agent.
Amber Lintner
November 2, 2025 AT 19:07Oh, the tragedy of dismissing cyproheptadine as mere “adjunct” when the nightmarish grip of insomnia and anorexia devours patients! This so‑called “antihistamine” becomes a hero in the shadows, rescuing the weary soul from endless agitation. The very notion that clinicians would shy away from its seductive promise is a calamity of epic proportion. Let the skeptics gnash their teeth; the evidence, though modest, screams louder than a chorus of dissenting voices. In the theater of depression treatment, cyproheptadine deserves a standing ovation.
Jennifer Stubbs
November 11, 2025 AT 01:07From a clinical standpoint, cyproheptadine’s antihistaminic and anti‑serotonergic actions can indeed address certain phenotypes of atypical depression, particularly those marked by hypersomnia and poor appetite. The anti‑inflammatory properties add another layer of plausibility, given the emerging link between cytokines and mood disorders. However, the modest sample sizes of the trials and the reliance on open‑label designs limit the generalizability of the findings. Physicians should weigh the sedative side‑effects against potential benefits, especially in patients already vulnerable to cognitive slowing. Ultimately, a personalized assessment remains the prudent path.
Veronica Appleton
November 19, 2025 AT 07:07Here are a few practical tips for anyone thinking about adding cyproheptadine to their regimen Start low 2 mg once daily and watch for drowsiness Increase slowly up to 4 mg twice daily if needed Monitor for dry mouth constipation and blurred vision especially in older adults Check other meds for CYP2D6 interactions Adjust doses accordingly Keep a symptom diary to track sleep appetite and mood changes This collaborative approach can help maximize benefit while minimizing risk
the sagar
November 27, 2025 AT 13:07Don’t be fooled by the Western pharma narrative that downplays cyproheptadine’s true potential.
Grace Silver
December 5, 2025 AT 19:07When one contemplates the intertwined pathways of histamine and serotonin, the mind wanders to the ancient notion of balance within the psyche. Cyproheptadine, by tempering both H1 and 5‑HT2 receptors, becomes a modern alchemist seeking that equilibrium. The sedative veil it casts over the restless brain can be likened to a gentle nightfall that quiets turbulent thoughts. In that quietude, neural circuits have the space to reconfigure toward a more harmonious rhythm. The appetite‑stimulating facet offers a corporeal reminder that nourishment and mood are inseparable companions. As the body receives sustenance, the brain receives a signal that survival is assured, easing existential dread. Inflammation, the silent fire that gnaws at synaptic fidelity, is dampened by the drug’s mast‑cell stabilization. By lowering cytokine spillover, the microglial landscape may shift from hostile to supportive. This anti‑inflammatory whisper aligns with emerging theories that view depression as a systemic illness. Moreover, the modulation of the HPA axis introduces a subtle regulation of stress hormones that often dominate depressive narratives. Lower cortisol surges grant the individual a reprieve from chronic fight‑or‑flight exhaustion. The paradox of an antihistamine acting as an antidepressant challenges the reductionist view that single‑target drugs suffice. It invites a broader contemplation of poly‑modal interventions that honor the brain’s complexity. Yet, the clinical data remain modest, a reminder that philosophical elegance does not guarantee therapeutic triumph. Practitioners must therefore balance wonder with rigor, embracing cyproheptadine where its multifaceted actions align with patient presentation. In the end, the drug serves as a testament to the imperfect but hopeful tapestry of modern psychopharmacology
Clinton Papenfus
December 14, 2025 AT 01:07Esteemed colleagues let us consider the disciplined application of cyproheptadine within a structured therapeutic protocol Initiate therapy with a modest dosage observe patient response after a fortnight and adjust accordingly Maintain rigorous documentation of side‑effects and concomitant medications Uphold the highest standards of clinical vigilance as we explore this adjunctive avenue Together we may elevate patient outcomes whilst honoring the sanctity of evidence based practice
Zaria Williams
December 22, 2025 AT 07:07Yo let me break it down for the masses – cyproheptadine ain’t no magic pill but it ain’t trash either. If you’re the type who chases every new hype you’ll probably overrate it, but if you’re stuck in a rut of insomnia and loss of appetite it can actually do some good. The studies are small but they show a real effect for the right crowd. Don’t let the “first‑line only” crowd boss you around – every med has its niche. Just don’t expect it to turn your life upside down overnight, fam.
ram kumar
December 30, 2025 AT 13:07Honestly i could barely muster the enthusiasm to type this but i guess i have to point out that the whole hype around cyproheptadine is just another circus act for bored psych docs. they sprinkle a few case reports and suddenly everyone acts like they discovered fire. sure it has some marginal benefits for a select few but the lazy pharma machine will sell it as a cure‑all while ignoring the yawning gaps in rigorous trials. i’m tired of watching endless debates that lead nowhere – it’s a drain on everyone’s energy.