Beta-Blockers: How Different Types Interact and Why Drug Choice Matters
 Dec, 2 2025
Dec, 2 2025
Beta-Blocker Selector
Which condition are you treating?
Do you have respiratory conditions?
Are you concerned about side effects?
Do you have diabetes?
Do you take other heart medications?
Recommended Beta-Blocker
Select your answers to see a personalized recommendation
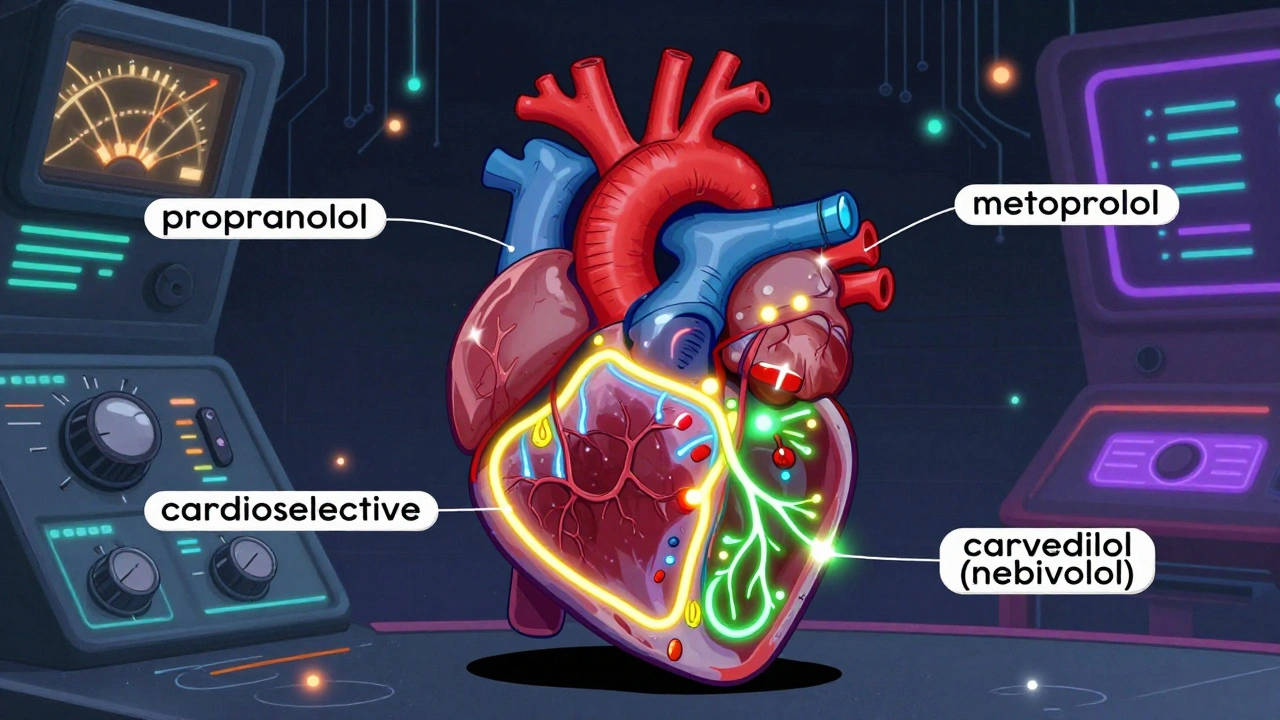
When you hear "beta-blocker," you might think of one drug-maybe metoprolol or propranolol. But the truth is, beta-blockers aren’t one-size-fits-all. There are beta-blockers that target only the heart, others that open blood vessels, and some that can make asthma worse. Choosing the right one isn’t just about the condition you have-it’s about your whole body, your other meds, and even your lifestyle.
What Beta-Blockers Actually Do
Beta-blockers work by blocking adrenaline and noradrenaline from binding to beta receptors in your heart and blood vessels. These are the chemicals your body releases when you’re stressed, scared, or exercising. When they bind, your heart beats faster, harder, and your blood pressure rises. Beta-blockers slow that down. That’s why they help with high blood pressure, irregular heartbeats, chest pain, and even migraines.
But here’s the catch: not all beta receptors are the same. There are three types-beta-1, beta-2, and beta-3. Beta-1 receptors are mostly in the heart. Beta-2 are in your lungs, blood vessels, and muscles. Beta-3 are involved in fat breakdown and blood vessel relaxation. The drugs you take determine which ones they block-and that makes all the difference.
The Three Generations of Beta-Blockers
Doctors group beta-blockers into three generations based on what they target and what extra effects they have.
First-generation drugs like propranolol and nadolol block both beta-1 and beta-2 receptors. That means they slow your heart-but they also tighten your airways. If you have asthma or COPD, this can be dangerous. These drugs were the first to be used, back in the 1960s, and they’re still around because they’re cheap. But they’re not the go-to anymore unless there’s a specific reason.
Second-generation beta-blockers like atenolol, bisoprolol, and metoprolol are more selective. They mostly stick to beta-1 receptors in the heart. That makes them safer for people with lung issues. Metoprolol comes in two forms: immediate-release (Lopressor), taken twice a day, and extended-release (Toprol XL), taken once. The extended version gives steadier levels, which means fewer side effects like fatigue or dizziness.
Third-generation drugs like carvedilol and nebivolol do something extra. Carvedilol also blocks alpha-1 receptors, which helps relax blood vessels. Nebivolol triggers your blood vessels to make more nitric oxide, a natural vasodilator. Both lower blood pressure not just by slowing the heart, but by opening up arteries. That’s why they’re the preferred choice for heart failure-especially when the heart’s pumping ability is weak.
Why Carvedilol and Nebivolol Stand Out in Heart Failure
If you’ve been diagnosed with heart failure with reduced ejection fraction (HFrEF), your doctor is likely to pick carvedilol or nebivolol. Why? Because they don’t just slow your heart-they protect it from damage over time.
Carvedilol reduces oxidative stress in heart muscle by 30-40% in lab studies. That means less scarring, less stiffening, and better long-term function. In the US Carvedilol Heart Failure Trial, patients taking carvedilol had a 35% lower risk of death compared to those on placebo. Nebivolol showed similar results in the SENIORS trial, cutting cardiovascular deaths by 14% in older adults.
These drugs also help with symptoms. People on carvedilol report less shortness of breath and fatigue over time. In a Cleveland Clinic survey, 85% of heart failure patients stuck with carvedilol because they felt better and had fewer breathing problems than with older beta-blockers.
But there’s a catch. Both require slow dose increases. Carvedilol starts at 3.125 mg twice daily and may take 8-16 weeks to reach the full 25 mg twice daily dose. Rush it, and you could get dizzy or faint. Nebivolol can be titrated faster, often reaching target doses in 4-8 weeks.
Side Effects: Not All Beta-Blockers Are Created Equal
Everyone worries about side effects. Fatigue, cold hands, slow heart rate-those are common. But the risk varies by drug.
Propranolol has a reputation for causing sleep problems and depression. On Drugs.com, 38% of users reported moderate to severe side effects, including 27% with insomnia and 19% with low mood. Metoprolol users report fatigue in 42% of cases and cold extremities in 29%. But bisoprolol? Only 18% report sleep issues and 11% depression. That’s a big difference.
There’s also a surprising benefit with nebivolol. In Reddit’s r/Cardiology community, 65% of men over 50 on nebivolol said their sexual function improved, compared to just 35% on older beta-blockers. That’s because nebivolol improves blood flow-not just to the heart, but everywhere. Other beta-blockers can reduce blood flow to the genitals, making erectile dysfunction worse.
And if you have asthma? Avoid nonselective beta-blockers like propranolol and sotalol. Even cardioselective ones like metoprolol can cause trouble at high doses. The European Medicines Agency warns that nonselective beta-blockers can cut the effect of asthma inhalers by 40-50%. That’s not worth the risk.
Why Beta-Blockers Are No Longer First-Line for High Blood Pressure
You might be surprised to learn that beta-blockers are no longer the top pick for simple high blood pressure. According to the Mayo Clinic’s 2023 guidelines, drugs like ACE inhibitors, ARBs, calcium channel blockers, and diuretics work better at lowering central aortic pressure-the pressure that actually stresses your heart and arteries.
Studies show beta-blockers lower central pressure by only 5-7 mmHg, while ACE inhibitors drop it by 10-12 mmHg. That’s why they’re now reserved for people with heart failure, post-heart attack, or arrhythmias-even if they also have high blood pressure.
But here’s the nuance: carvedilol and nebivolol still work well for hypertension because of their vasodilating effects. They can drop systolic pressure by an extra 10-15 mmHg compared to older beta-blockers. So if you’re on a beta-blocker for blood pressure, it’s likely because you have another condition that makes it the best fit.
What Happens If You Stop Suddenly?
Never stop a beta-blocker cold turkey. The FDA issued a warning in 2021: abruptly stopping these drugs can triple your risk of heart attack in the first 48 hours. Why? Your body has adapted to the drug. When you pull it away, adrenaline surges back unchecked. Your heart rate spikes, blood pressure rockets, and your heart can’t handle the shock.
If you need to stop-for surgery, side effects, or other reasons-your doctor will taper you down slowly, often over 1-2 weeks. Skipping doses or cutting pills in half without guidance is dangerous.
How to Know Which One Is Right for You
There’s no single best beta-blocker. The right one depends on:
- What condition you’re treating (heart failure? arrhythmia? migraine?)
- Whether you have asthma, COPD, or diabetes
- Other medications you take (like antidepressants or insulin)
- Your age and kidney function
- Whether you’re concerned about fatigue or sexual side effects
For heart failure: carvedilol or nebivolol. For post-heart attack: bisoprolol or metoprolol succinate. For tremors or anxiety: propranolol still has a role. For high blood pressure alone: skip beta-blockers unless you have another reason.
The American College of Cardiology offers a free "Beta-Blocker Selection Toolkit" that helps doctors weigh 12 factors-from kidney function to drug interactions-to pick the best fit. It’s not guesswork anymore.
What’s Coming Next?
Research is moving fast. In 2023, the FDA approved entricarone-a new drug that blocks beta-1 receptors while activating beta-3 receptors-for heart failure with preserved ejection fraction. Early results show a 22% drop in hospitalizations.
By 2024, a combination pill of nebivolol and valsartan (an ARB) will hit the market, offering dual protection in one tablet. And in the GENETIC-BB trial, researchers are testing whether your DNA can predict which beta-blocker you’ll respond to best. Imagine a blood test telling you: "You’ll do better on carvedilol than metoprolol." That’s the future.
For now, the message is clear: beta-blockers are powerful-but only when chosen wisely. The difference between a drug that saves your life and one that just makes you tired comes down to the details. Talk to your doctor about which one fits your body, not just your diagnosis.
Are all beta-blockers the same?
No. Beta-blockers vary by selectivity (beta-1 vs. beta-2 receptors), duration of action, and extra effects like vasodilation. Carvedilol and nebivolol have added benefits for heart failure, while propranolol can worsen asthma. The drug you take matters as much as the condition being treated.
Which beta-blocker is safest for someone with asthma?
Cardioselective beta-blockers like bisoprolol, metoprolol, or atenolol are safer than nonselective ones like propranolol. But even these can cause breathing issues at high doses. Always use the lowest effective dose and avoid them if you have severe asthma. Nebivolol may be the safest option due to its nitric oxide effect, which can help open airways slightly.
Why is carvedilol preferred over metoprolol for heart failure?
Carvedilol blocks both beta and alpha receptors, reducing heart strain and relaxing blood vessels. It also lowers oxidative stress in heart tissue by 30-40%, which helps prevent long-term damage. In clinical trials, carvedilol reduced death risk by 35% compared to placebo, while metoprolol tartrate showed a smaller benefit. Metoprolol succinate (extended-release) is also effective, but carvedilol has broader protective effects.
Can beta-blockers cause depression or fatigue?
Yes, especially with older drugs like propranolol. Up to 19% of users report depression, and 42% feel fatigued. Newer agents like bisoprolol and nebivolol have lower rates-around 11-18%. Fatigue often improves after a few weeks as your body adjusts. If side effects persist, talk to your doctor about switching to a different beta-blocker.
Is it safe to take beta-blockers with other heart meds?
Yes, but carefully. Beta-blockers are often combined with ACE inhibitors, ARBs, diuretics, and SGLT2 inhibitors in heart failure. But combining them with calcium channel blockers like diltiazem or verapamil can cause dangerously slow heart rates. Always tell your doctor about every medication, including over-the-counter supplements like St. John’s wort, which can interfere with metabolism.
Do beta-blockers affect blood sugar?
Yes. Beta-blockers can mask symptoms of low blood sugar like rapid heartbeat and shakiness. They may also slightly raise blood sugar levels, especially nonselective ones. Diabetics on beta-blockers should monitor glucose more closely and inform their doctor if they notice unusual patterns.
If you’re on a beta-blocker, don’t assume all of them work the same. The right choice depends on your heart, your lungs, your other meds, and even your quality of life. Ask your doctor: "Why this one?" and "Is there a better fit?" Your body will thank you.
James Kerr
December 3, 2025 AT 07:28Been on metoprolol for years-fatigue was brutal at first, but after 3 weeks it smoothed out. Still get cold hands though. 🤷♂️
Chloe Madison
December 3, 2025 AT 20:02So many people think beta-blockers are just "heart pills"-but the difference between carvedilol and propranolol is like comparing a sports car to a tractor. One gets you where you need to go with grace. The other? You feel every bump. And if you’ve got asthma? Propranolol is a hard no. Your lungs will thank you.
I’ve seen patients switch from metoprolol to nebivolol and suddenly they’re walking their dogs again without gasping. It’s not magic-it’s pharmacology. Nebivolol’s nitric oxide boost? That’s the secret sauce for blood flow, not just the heart.
And don’t even get me started on stopping cold turkey. I had a patient who quit because he thought it "wasn’t working"-woke up in the ER with a heart rate of 152. Never again. Taper. Slow. Smart.
Also, if you’re a guy over 50 and your sex life tanked after starting a beta-blocker? Try switching to nebivolol. It’s not just a myth-65% of men in r/Cardiology say it helped. Other beta-blockers? They can shut down circulation everywhere. Nebivolol opens it up. That’s huge.
And yes, they’re not first-line for simple hypertension anymore. But if you’ve got heart failure, post-MI, or arrhythmia? These drugs are lifesavers. Just pick the right one. Your body isn’t a spreadsheet-it’s a symphony. And every drug plays a different instrument.
Makenzie Keely
December 4, 2025 AT 11:17Let’s be crystal-clear: not all beta-blockers are created equal-and this is not a minor detail. It’s a life-or-death distinction. Propranolol? Nonselective. Blocks beta-1 AND beta-2. That means it can constrict your airways-potentially triggering a life-threatening asthma attack. Even at low doses. The EMA warned about this. Yet, some doctors still prescribe it out of habit.
Meanwhile, nebivolol? It’s a third-generation marvel. Not only is it cardioselective, but it also stimulates endothelial nitric oxide synthase. That means vasodilation. That means less peripheral resistance. That means better outcomes in elderly patients with heart failure. The SENIORS trial? 14% reduction in cardiovascular death. That’s not a footnote-it’s a headline.
And carvedilol? It’s an alpha-1 blocker too. So it doesn’t just slow the heart-it relaxes the arteries. That’s why it’s preferred in HFrEF. And yes, the dose titration is slow-but that’s not a flaw, it’s a feature. Rushing it leads to hypotension, syncope, and hospitalization. Patience is part of the treatment.
Also-fatigue? Depression? Yes, they happen. But they’re not universal. Bisoprolol has the lowest incidence of mood-related side effects. Metoprolol tartrate? Higher. Propranolol? Highest. This isn’t random. It’s pharmacokinetics. And if your doctor prescribes propranolol for anxiety and you’re a diabetic? They’re not thinking about masked hypoglycemia. That’s negligence.
Bottom line: if you’re on a beta-blocker, ask your doctor: "Which receptor subtype does this target?" If they can’t answer, it’s time to find a new one. This isn’t guesswork. It’s precision medicine.
bobby chandra
December 5, 2025 AT 03:31Yo, beta-blockers are like different types of coffee. Propranolol? That bitter, black, 4am espresso that gives you jitters and insomnia. Metoprolol? The medium roast-works fine but makes you sluggish. Nebivolol? That smooth, latte-with-a-hint-of-vanilla version that actually makes you feel… good. Carvedilol? The cold brew with extra antioxidants. You don’t just drink coffee for caffeine-you drink it for the vibe. Same with beta-blockers. Pick the one that doesn’t turn your life into a zombie movie.
And yeah, I got my ED fixed by switching from metoprolol to nebivolol. No joke. My wife noticed. My doctor was like, "Huh, that’s not supposed to happen." Turns out, nitric oxide doesn’t just help your heart-it helps your… other organs. Who knew?
Also-never quit cold turkey. I saw a dude try it after reading a Reddit post. He ended up in the ER with a heart attack. Don’t be that guy. Taper. Like your life depends on it. Because it does.
shalini vaishnav
December 5, 2025 AT 08:26Western medicine is so obsessed with "precision" it forgets the basics. In India, we treat hypertension with diet, yoga, and ajwain water. Beta-blockers? Only for emergencies. You think your heart is fragile because you sit at a desk? We’ve been alive for centuries without these pills. Your body doesn’t need to be chemically tamed-it needs to be strengthened. These drugs are corporate inventions disguised as science.
vinoth kumar
December 5, 2025 AT 22:37Hey, I’m from India and I’ve been on carvedilol for 2 years after my MI. Honestly? Best decision I ever made. My ejection fraction went from 32% to 51%. No magic, just science. And yeah, I had to start at 3.125mg-felt like a ghost for 2 weeks. But now? I walk 8km daily. No shortness of breath. My doctor told me it’s because carvedilol protects the heart muscle. Not just slows it. That’s the difference.
Also, my sugar levels were weird at first. Beta-blockers hide hypoglycemia. So I started checking my glucose twice a day. Small change. Big difference.
Ignacio Pacheco
December 7, 2025 AT 08:34So… let me get this straight. We’ve got a class of drugs that can kill you if you stop them cold turkey, cause depression, erectile dysfunction, and fatigue… but we’re still prescribing them like they’re Advil? And the reason? Because some trial from 2003 says they "reduce mortality"? Meanwhile, we’ve got people on nebivolol who report better sex lives and less fatigue. But your doctor still gives you metoprolol because it’s cheaper? Yeah. That’s not medicine. That’s capitalism with a stethoscope.
Gene Linetsky
December 7, 2025 AT 20:44They’re hiding the truth. Beta-blockers were pushed hard by Big Pharma after the 1980s because they were profitable. But the real reason they’re still around? Because the FDA doesn’t want to admit they approved drugs based on flawed trials. Look at the ALLHAT study. Beta-blockers underperformed diuretics for hypertension. But you don’t hear that on TV. Why? Because the drug reps still visit your doctor. And they don’t care if you get fatigued. They care about the quarterly report.
And nebivolol? That’s just a rebrand. Nitric oxide? Yeah, cool. But it’s still a beta-blocker. Same side effects. Same withdrawal risks. They just added a fancy label and called it "innovation."
And don’t even get me started on the "free toolkit" from the ACC. That’s not a tool. That’s a marketing brochure. They’re selling you a pill, not a solution.
Archie singh
December 8, 2025 AT 14:27Ugh. Another overcomplicated article written by someone who thinks "beta-1 receptor selectivity" is a personality trait. You don’t need a 2000-word essay to say "don’t take propranolol if you have asthma." It’s basic. Why is this even a conversation? You want to live? Don’t be dumb. Take the right pill. Done.
Vincent Soldja
December 10, 2025 AT 04:01Interesting. But I’m on metoprolol and it’s fine. No need for all this detail.
Jim Schultz
December 11, 2025 AT 19:15Wait-so you’re telling me that nebivolol improves sexual function? And carvedilol reduces oxidative stress? And bisoprolol has fewer mood side effects? And propranolol is basically a slow poison for asthmatics? And you’re telling me this isn’t common knowledge? Why are doctors still prescribing propranolol like it’s 1978? This isn’t just negligence. It’s malpractice. And the fact that you need a "toolkit" to pick the right one? That’s a system failure. Not a medical one.
Someone should sue the pharmaceutical companies for not updating guidelines faster. And the FDA for letting outdated drugs stay on the market while newer, safer ones are priced like luxury cars. This isn’t healthcare. It’s a rigged game.
Kidar Saleh
December 13, 2025 AT 05:17As a cardiologist in London, I’ve seen the shift firsthand. Ten years ago, metoprolol was the default. Now? Carvedilol and nebivolol are first-choice for heart failure. Why? Because the data doesn’t lie. But what’s more striking is how patients respond-not just physiologically, but emotionally. One man told me, "I didn’t know I could breathe again until I switched." That’s not just medicine. That’s dignity restored.
And yes, the tapering is painful. The fatigue is real. But so is the alternative: sudden cardiac death. This isn’t about convenience. It’s about survival. And if your doctor isn’t discussing the differences between beta-blockers with you? Ask again. And again. Until they listen.