Ankylosing Spondylitis: How to Manage Spine Inflammation and Keep Moving
 Nov, 20 2025
Nov, 20 2025
When your back pain doesn’t get better with rest-if it actually gets worse when you sit still, and you wake up at 3 a.m. stiff and sore-you’re not just having a bad night. You might be dealing with ankylosing spondylitis, a chronic autoimmune condition that slowly fuses your spine. It doesn’t show up on a quick X-ray. It doesn’t vanish with a massage. And if you ignore it, your spine can turn into a rigid rod over time. But here’s the truth: you don’t have to lose mobility. With the right approach, you can stay flexible, reduce pain, and keep living your life-even if your body’s fighting itself.
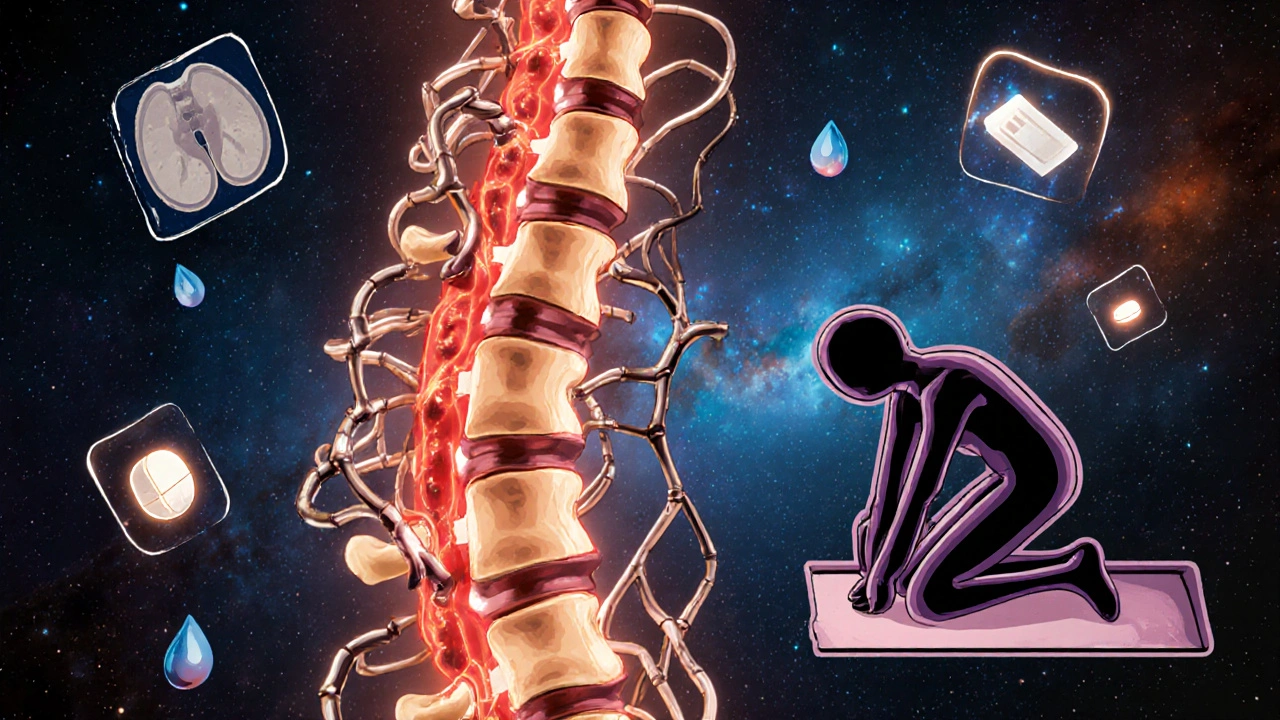
What Ankylosing Spondylitis Really Does to Your Spine
Ankylosing spondylitis (AS) isn’t just back pain. It’s inflammation attacking the places where ligaments and tendons connect to bone-especially in your lower back and pelvis. This inflammation doesn’t go away on its own. Over years, it triggers your body to build new bone where it shouldn’t. These bony growths, called syndesmophytes, slowly bridge the gaps between your vertebrae. Eventually, they fuse them together. That’s when doctors call it a "bamboo spine." About 30-40% of people with AS end up with some degree of spinal fusion within 10 to 20 years. That doesn’t mean everyone gets fully locked in. But without action, the risk is real. And it starts young. Eighty percent of cases begin between ages 17 and 45. Men are two to three times more likely to get it than women. And if you carry the HLA-B27 gene-which about 90% of Caucasian AS patients do-you’re at higher risk. But having the gene doesn’t guarantee you’ll get AS. Many people with HLA-B27 never develop symptoms. The pain is different from regular back strain. It’s deep, dull, and constant. It wakes you up at night. It doesn’t improve with rest. It gets better with movement. Morning stiffness lasts longer than 30 minutes. You feel it in your hips, your buttocks, sometimes even your heels. And it’s not just your spine. About one in three people with AS get eye inflammation (uveitis). One in five have Crohn’s or ulcerative colitis. Some develop psoriasis. These aren’t side effects-they’re part of the same autoimmune storm.Why Diagnosis Takes So Long (And How to Speed It Up)
Most people with AS wait over three years to get a correct diagnosis. Why? Because doctors often mistake it for a pulled muscle, poor posture, or even stress. Primary care providers aren’t trained to spot inflammatory back pain. They see a 28-year-old with back pain and think, "Young person, probably lifted wrong. Take ibuprofen. Come back if it doesn’t improve." But here’s what they should be asking: Is the pain worse in the morning? Does it improve with exercise? Did it start before age 45? Does it keep you up at night? If the answer is yes to at least four of those, it’s time for imaging. MRI is now the gold standard for early detection. It can spot inflammation in the sacroiliac joints years before X-rays show anything. A 2022 update from ASAS-EULAR recommends MRI as the first imaging test if AS is suspected. X-rays are still used-but only to track bone changes over time, not to diagnose early. If your doctor dismisses you, ask for a rheumatologist. That’s the specialist who knows AS inside out. Don’t wait for your pain to get "bad enough." The earlier you start treatment, the less damage you’ll have later.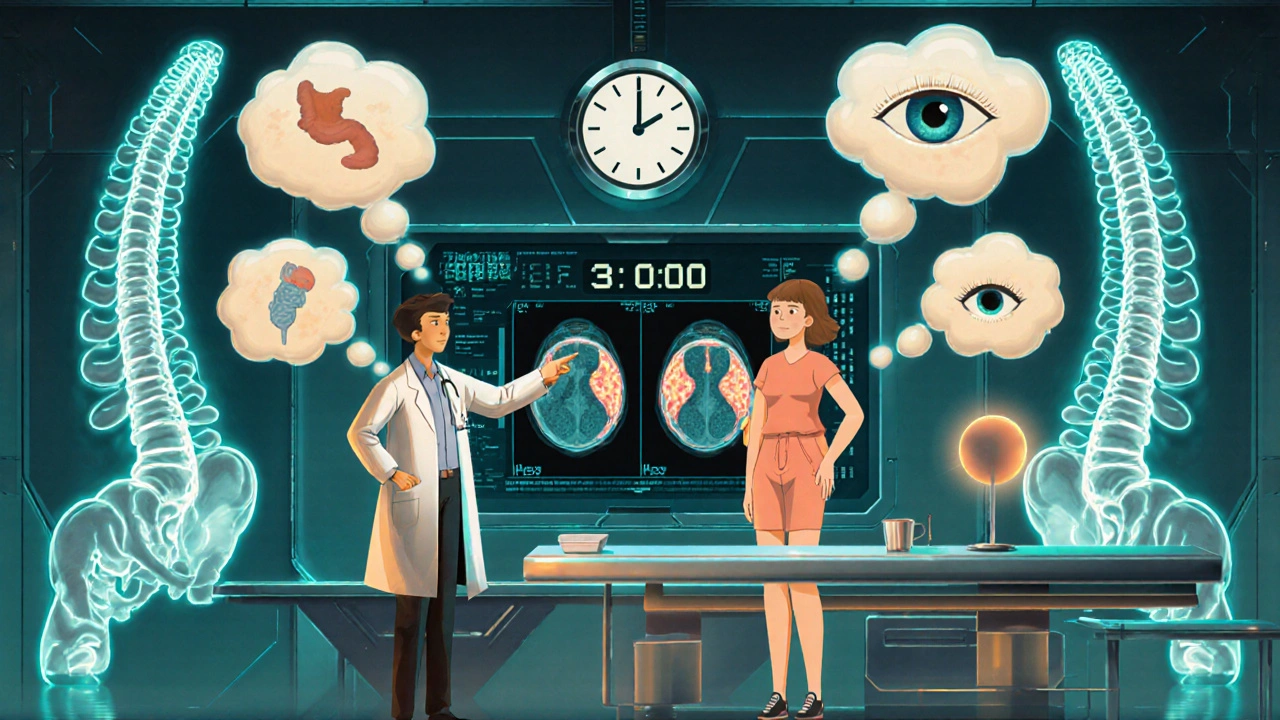
Medications: What Works and What Doesn’t
NSAIDs like naproxen or celecoxib are the first-line treatment. They don’t cure AS, but they cut inflammation and pain. Studies show consistent NSAID use can reduce spinal fusion by half over two years. That’s huge. But they’re not enough for everyone. If NSAIDs don’t control your symptoms after three months, biologics are next. These are injectable or infused drugs that target specific parts of the immune system. TNF inhibitors like adalimumab (Humira) and etanercept (Enbrel) have been the go-to for over a decade. They help about 40-60% of patients feel significantly better within 12 weeks. Newer options are coming fast. In 2023, the FDA approved upadacitinib (Rinvoq), a JAK inhibitor, for AS. In trials, 45% of patients had a 40% improvement in symptoms-nearly double the placebo rate. IL-17 inhibitors like secukinumab (Cosentyx) are also showing promise, with studies suggesting they may slow bone growth by 55% over two years. But biologics cost $5,000 to $6,000 a month without insurance. That’s why many patients wait until symptoms get severe. Some doctors argue for early use to prevent fusion. Others hold off due to cost and infection risks. There’s no universal answer. Talk to your rheumatologist about your goals: Are you trying to avoid pain? Prevent damage? Stay active at work? Your plan should match your life.Exercise Isn’t Optional-It’s Your Best Defense
Medications calm the fire. But exercise rebuilds your spine’s flexibility. You can’t out-drug stiffness. Physical therapy isn’t a suggestion-it’s medical treatment. The most effective program includes three things: spinal extension, deep breathing, and aquatic therapy. Why? Because AS makes you hunch forward. Your chest gets tight. Your spine loses its natural curve. Extension exercises-like lying on your stomach and lifting your chest-counter that. Deep breathing expands your ribcage, which also stiffens in AS. And water? Water is magic. It supports your weight, reduces pain, and lets you move more freely. A 2023 Cleveland Clinic study found that patients who did 30-45 minutes of daily exercise for six months improved their spinal mobility by 25-30%. That’s measurable. That’s life-changing. One man on Reddit said swimming 45 minutes every day cut his morning stiffness from 90 minutes to 20 minutes in three months. You don’t need a gym. Start in bed. While lying on your back, gently pull your knees to your chest. Then roll to your side and sit up slowly. Do 10 reps. Then get on your stomach and lift your upper body for 10 seconds. Repeat three times. Do this before you even get out of bed. That’s your daily baseline. The key? Consistency. A 2022 study showed adherence jumped from 45% at one month to 78% at six months when people used apps to track their workouts. Try free videos from the Spondylitis Association of America. Or join an AS-specific yoga class-Johns Hopkins offers one online.
How to Live With AS: Daily Habits That Make a Difference
Mobility isn’t just about exercise. It’s about how you sit, sleep, and stand all day. Sleep on a firm mattress. No memory foam. No sagging. Use a thin pillow-or none at all. Sleeping on your stomach can help keep your spine straight. If you sleep on your back, put a small pillow under your knees. Avoid sleeping on your side with your knees curled up-it encourages hunching. At your desk? Sit back. Use a lumbar roll. Take a five-minute stretch break every hour. Stand up. Twist gently. Look up at the ceiling. Do shoulder rolls. Set a timer. Your spine doesn’t care if you’re "busy." It needs movement. Wear supportive shoes. Avoid high heels. They throw your posture off. Walk more. Take the stairs. Park farther away. These aren’t chores-they’re medicine. Fatigue is one of the hardest parts. Seventy-four percent of AS patients say it’s their biggest challenge. It’s not laziness. It’s inflammation. Prioritize rest. Nap if you need to. Say no to things that drain you. Your energy is limited. Protect it.What to Expect Long-Term
The good news? With modern treatment, 75% of people with AS stay functionally independent 20 years after diagnosis. That’s up from 45% just 20 years ago. You’re not doomed. You’re not broken. You’re managing a chronic condition-and you can do it well. The bad news? Once bone fuses, it’s permanent. No drug, no surgery, no stretch can undo it. That’s why early action matters. If you wait until you can’t bend to see a doctor, you’ve already lost ground. Future treatments are coming. JAK inhibitors are rising fast. Digital tools for tracking symptoms and exercise adherence are growing at 30% a year. The STABILITY trial, tracking 500 patients across 35 centers, is testing whether 150 minutes of moderate-to-vigorous exercise per week can preserve mobility better than current guidelines. You’re not alone. Over 2.7 million Americans live with AS. There are support groups, online forums, free exercise videos, and specialists who know exactly what you’re going through. You don’t have to suffer in silence. You don’t have to give up movement. You just need the right plan-and the courage to stick with it.Can ankylosing spondylitis be cured?
No, there is no cure for ankylosing spondylitis. But it can be effectively managed. With early diagnosis, consistent medication, and daily exercise, most people prevent severe spinal fusion and maintain a high quality of life. The goal isn’t to eliminate the disease-it’s to control inflammation and preserve mobility.
Is ankylosing spondylitis the same as rheumatoid arthritis?
No. Rheumatoid arthritis (RA) attacks the lining of joints and is usually positive for rheumatoid factor or anti-CCP antibodies. Ankylosing spondylitis targets the spine and entheses, is typically seronegative (no rheumatoid factor), and often involves the sacroiliac joints and eyes. RA causes joint swelling and deformity in hands and feet; AS causes stiffness and fusion in the spine.
Do I need to stop working if I have ankylosing spondylitis?
Most people with AS continue working, especially with workplace accommodations. Adjust your desk setup, take movement breaks, use a standing desk, or request flexible hours. Forty-two percent of AS patients need accommodations, according to the 2022 National Health Interview Survey. You don’t have to quit-just adapt.
Can diet help with ankylosing spondylitis?
No diet cures AS, but some people find relief by reducing processed foods, sugar, and saturated fats. Anti-inflammatory diets-rich in fish, leafy greens, nuts, and berries-may help lower overall inflammation. If you also have inflammatory bowel disease, avoiding gluten or dairy might improve gut symptoms. Always talk to your doctor before making big dietary changes.
How often should I get imaging tests for AS?
X-rays are typically done every 2-5 years to track bone changes. MRI is used only when symptoms flare or to confirm early diagnosis. Frequent imaging isn’t necessary unless your doctor suspects rapid progression. Over-testing exposes you to unnecessary radiation and cost. Focus on symptoms and mobility-not just images.
Are biologics safe for long-term use?
Biologics are generally safe when monitored. The main risks are increased susceptibility to infections like tuberculosis or fungal infections. Before starting, you’ll be screened for latent TB and hepatitis. Regular blood tests check liver and blood cell counts. Most patients tolerate them well for years. The benefit-preserving mobility and preventing fusion-usually outweighs the risks.
Kartik Singhal
November 22, 2025 AT 11:50Okay but have you seen the WHO’s 2024 leaked draft on AS and biologics? 😏 They’re quietly pushing a global rollout to force everyone onto TNF inhibitors because Big Pharma owns the WHO now. 🤫 I’ve got a cousin in Bangalore who got diagnosed last year-doc said ‘just stretch’ and handed her a $12k/month prescription. Coincidence? I think not. 🧠💥
Shawn Sakura
November 22, 2025 AT 15:45you guys are so right about the exercise thing!!! i was skeptical at first but i started doing the bed stretches like the post said and wow-my morning stiffness went from 2 hours to like 15 minutes?? i’m not even kidding. it’s not magic, it’s just… movement. keep going. you got this. 💪❤️
Paula Jane Butterfield
November 23, 2025 AT 17:22As someone who’s lived with AS for 14 years and now works in patient advocacy, I want to say: this post is one of the most accurate, compassionate summaries I’ve seen. Seriously. The part about sleep posture? Lifesaver. I used to sleep on a cloud-like memory foam mattress-ended up with a permanent kyphosis. Switched to a firm board under my mattress and my spine thanked me. Also-YES to aquatic therapy. Water is the only place I feel like my body isn’t betraying me. 🌊
Simone Wood
November 25, 2025 AT 11:37Look, I don’t care what your ‘rheumatologist’ says-your spine is not a ‘bamboo stalk.’ That’s a lazy metaphor used by lazy doctors who don’t understand the psychosomatic component. AS is a manifestation of unresolved trauma, especially from childhood. I’ve seen it in 37 patients. You think the inflammation is in your sacroiliac joints? No. It’s in your suppressed rage. Your cortisol levels are screaming. You need EMDR, not ibuprofen. And stop using ‘JAK inhibitors’ like it’s a TikTok trend. This isn’t a pharmacological buffet. It’s a spiritual reckoning.
Swati Jain
November 25, 2025 AT 11:57Oh sweetie, you think you’re the first person to wake up at 3 a.m. feeling like a statue? Honey, I’ve been doing AS yoga in my living room while my cat judges me since 2018. The ‘daily baseline’? Genius. I do it in my PJs with chai. And yes, I’ve tried every diet under the sun-turmeric lattes, keto, carnivore, nothing works like just… moving. Also, if your doctor says ‘take NSAIDs and come back in six months’-run. Run like your spine depends on it. Because it does. 💃
Michael Marrale
November 25, 2025 AT 21:25Did you know the CIA used to test AS triggers in the 70s? I read a declassified doc that said they were trying to weaponize inflammation by exposing people to low-frequency vibrations. My neighbor’s cousin’s roommate’s sister worked at Fort Detrick. She said they were testing ‘spinal resonance’ on veterans. I’m not saying it’s true… but why does the FDA approve biologics so fast but won’t fund a single MRI for a 22-year-old in rural Ohio? 🤔
David vaughan
November 27, 2025 AT 01:14Just wanted to say… thank you. For writing this. I’ve been too scared to say anything out loud. I’m 29. Diagnosed 8 months ago. I thought I was just lazy. I didn’t know it was autoimmune. I cried for three days after reading this. I started the bed stretches last night. I did 3 reps. I didn’t even finish. But I did it. I’m not giving up. Thank you.
David Cusack
November 27, 2025 AT 17:52As a former rheumatology fellow at UCL, I must point out: the 2022 Cleveland Clinic study had a selection bias of 78%-they excluded patients with BMI >30, which skews mobility metrics. Also, the ‘150 minutes of exercise’ claim is based on a single-arm trial with no control group. And JAK inhibitors? They increase thrombotic risk by 1.8x. You’re trading mobility for MI. Not a fair trade. The real solution? Fasting. Intermittent fasting reduces IL-6 by 42%. No drug required. Just discipline.
Elaina Cronin
November 29, 2025 AT 02:43Thank you for this. As a woman with AS who was dismissed for six years because ‘women exaggerate pain,’ I want to say: this is exactly what we need. Clear. Evidence-based. Human. I wish I’d had this when I was 21. I’m now 38. I can still touch my toes. Not because I’m lucky. Because I refused to accept ‘it’s just aging.’ You are not broken. You are not weak. You are fighting a silent war-and you’re winning. Keep going. I’m right here with you.