Aging & Bone Health: Proven Tips to Keep Bones Strong
 Oct, 3 2025
Oct, 3 2025
Bone Health Risk Assessment
Assessment Questions
Answer the following questions to assess your bone health risk level.
Your assessment results will appear here
As we get older, the skeleton that once felt indestructible can start to lose density, making everyday activities feel riskier. Understanding why bone health and age are tangled together is the first step toward keeping your frame sturdy well into your senior years.
TL;DR
- Bone loss speeds up after age 50, especially for women.
- Calcium, vitamin D, and weight‑bearing exercise are the top natural defenses.
- Screen for osteoporosis with a bone density test starting at 65 (or earlier if risk factors exist).
- Quit smoking, limit alcohol, and maintain a healthy weight.
- Create a simple weekly plan that mixes strength, balance, and cardio.
Why Bones Change with Age
When you hear the term Aging the natural, progressive decline in physiological functions that begins in early adulthood you might picture wrinkles, not weak skeletons. Yet the same hormonal shifts, reduced cellular turnover, and slower absorption of nutrients that affect skin also impact bone tissue.
Two processes dominate:
- Bone remodeling slowdown: Young adults replace about 10% of their bone each year. After the mid‑30s, the balance tips toward resorption, meaning more bone is broken down than rebuilt.
- Loss of bone mineral density (BMD): Measured in grams per square centimeter, BMD drops roughly 1% per year after age 40, accelerating to 2% after menopause for women.
These changes set the stage for Osteoporosis a disease characterized by porous, fragile bones and an increased risk of fractures, the most common bone‑related condition in adults over 65.
Key Risk Factors You Can Control
Not all aging‑related bone loss is inevitable. Several lifestyle choices tip the scales:
- Smoking: Nicotine reduces calcium absorption and impairs hormone production.
- Excessive alcohol (>3 drinks/day): Interferes with vitamin D metabolism.
- Low body weight: Less mechanical load means less stimulus for bone formation.
- Lack of physical activity: Sedentary habits deprive bones of the stress they need to stay strong.
- Inadequate nutrition: Deficiencies in calcium, vitamin D, magnesium, and vitamin K2 undermine mineralization.
Women also face the hormonal dip of Menopause the period marking the end of menstrual cycles, typically around age 51, which sharply lowers estrogen levels. Estrogen protects bone by limiting resorption, so its loss can cause a rapid BMD decline.
Nutrition That Powers Strong Bones
Think of bone as a living tissue that needs a steady supply of minerals and vitamins. While calcium gets most of the spotlight, a balanced mix delivers the best results.
| Nutrient | RDA (Adults) | Top Food Sources | Bone Role |
|---|---|---|---|
| Calcium | 1,000mg (women<50, men<70); 1,200mg (women≥50, men≥70) | Dairy, fortified plant milks, leafy greens (kale, bok choy) | Provides the mineral matrix that makes bone rigid. |
| VitaminD | 800-1,000IU | Fatty fish, egg yolks, sunlight‑triggered synthesis in skin | Boosts calcium absorption in the gut. |
| Magnesium | 310-420mg | Almonds, black beans, whole grains | Activates vitaminD and influences bone crystal formation. |
| VitaminK2 | 90-120µg | Natty cheeses, fermented soy (natto) | Guides calcium to bone rather than arteries. |
| Phosphorus | 700mg | Meat, dairy, nuts | Works with calcium to form hydroxyapatite crystals. |
Putting these foods on a plate is easier than counting pills, but a supplement regimen can fill gaps. The most evidence‑based combos are calcium+vitaminD, and magnesium+vitaminK2 for older adults who struggle with dietary intake.
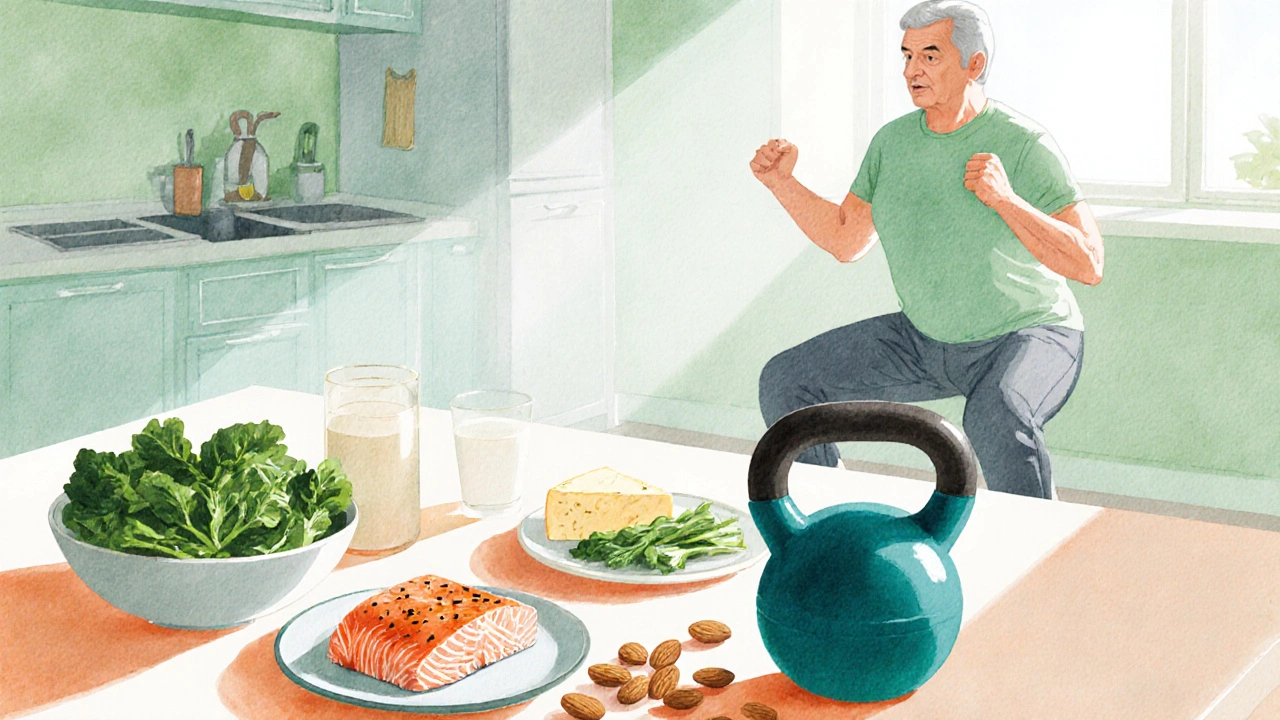
Exercise Strategies for Every Age
Bone responds to mechanical load-a principle called Wolff’s Law. The more you challenge your skeleton, the more it reinforces itself.
Weight‑bearing exercise any activity where you stand upright and support your own weight, such as walking, jogging, or resistance training is the gold standard. Aim for at least 150 minutes of moderate‑intensity cardio plus two strength‑training sessions per week.
Here’s a simple weekly template:
- Monday - 30min brisk walk (moderate intensity).
- Tuesday - 20min resistance circuit (bodyweight squats, lunges, push‑ups).
- Wednesday - Rest or gentle yoga for balance.
- Thursday - 30min interval jogging (1min fast, 2min easy).
- Friday - 20min resistance with dumbbells (deadlifts, shoulder press).
- Saturday - 45min hiking or dancing.
- Sunday - Light stretching or tai chi.
Include balance work (tai chi, single‑leg stands) to prevent falls-a leading cause of fracture in seniors.
Screening & Medical Options
Knowing your bone density lets you act before a fracture occurs. The standard test is the Bone density test also called a DXA scan, which measures bone mineral density using low‑dose X‑rays. Guidelines suggest:
- Women≥65 and men≥70 get a baseline scan.
- Anyone with risk factors (early menopause, long‑term steroids, family history) should screen at 50.
If results show a T‑score ≤‑2.5, doctors may prescribe anti‑resorptive meds like bisphosphonates or newer agents such as denosumab. Hormone‑replacement therapy can also protect bone in early post‑menopausal women, but it requires individualized risk assessment.
For those with osteopenia (T‑score between ‑1.0 and ‑2.5), lifestyle changes alone often suffice, but regular monitoring every 2-3years is wise.
Building Your Personal Bone‑Health Plan
Turn the info above into a concrete routine:
- Assess risk: List family history, menopause age, medication use, and current activity level.
- Schedule a DXA scan if you meet age or risk criteria.
- Set nutrition goals: Aim for 1,200mg calcium and 1,000IU vitaminD daily; add magnesium and vitaminK2.
- Choose a workout mix: Combine three days of weight‑bearing cardio, two days of resistance, and two balance/flexibility sessions.
- Track progress: Use a simple journal or app to note food, supplement doses, and exercise minutes.
- Review annually: Re‑check BMD, revisit supplements, and adjust intensity as fitness improves.
Sticking to this plan reduces fracture risk by up to 40% according to the National Osteoporosis Foundation’s 2024 data.
Frequently Asked Questions
How often should I get a bone density test?
Women 65+ and men 70+ should have a DXA scan every two years. If you have risk factors-early menopause, chronic steroid use, or a family history of fractures-start at age 50 and repeat every 1-2years.
Can I get enough calcium from food alone?
Most adults can meet the RDA with dairy or fortified plant milks, plus leafy greens. If you avoid these foods, a calcium supplement (500‑600mg) taken with vitaminD is a reliable backup.
Is weight‑bearing exercise safe if I have knee arthritis?
Low‑impact options like brisk walking, elliptical training, or water aerobics still provide the mechanical load bones need without over‑stressing joints. Pair with strength work for the surrounding muscles to improve joint stability.
Do men need as much calcium as women?
Yes. Men lose bone density at a similar rate after their 30s, and the same RDA (1,000mg under 70, 1,200mg over 70) applies.
What role does vitaminK2 play in bone health?
VitaminK2 activates osteocalcin, a protein that locks calcium into the bone matrix, preventing it from depositing in arteries. Studies show a 15‑20% reduction in fracture risk when vitaminK2 intake meets the RDA.
Dawson Turcott
October 3, 2025 AT 05:40Wow, who knew that chugging milk and doing a few push‑ups could turn you into a bone‑like superhero? 😂 It’s almost like the universe is handing out cheat codes for osteoporosis if you just remember to snack on cheese and walk up the stairs instead of the elevator. Sure, you could also just keep smoking and drinking, but then you’ll be the living proof that “you can’t have your cake and eat it too” applies to calcium too. Anyway, keep those vitamins coming and maybe you’ll outrun the frailty police. 🙄
Alex Jhonson
October 15, 2025 AT 23:14Hey folks, just wanted to add a splash of color to the conversation – think of your bones as the scaffolding of a vibrant mural. A daily dose of leafy greens, a sprinkle of sunshine for vitamin D, and a regular stroll can keep that masterpiece from cracking. Remember, even the brightest hues need a solid base, so don’t skip the dairy or fortified alternatives. Stay kind to your body, and it’ll return the favor with a sturdy frame for all your adventures. 🌈
Katheryn Cochrane
October 28, 2025 AT 15:47Let’s cut the fluff – most of these “tips” are just rehashed health propaganda. You’re told to drink milk, take calcium, do cardio – it’s a one‑size‑fits‑none approach. The real problem is the industry that pushes supplements while ignoring socioeconomic barriers. If you can’t afford fresh produce, suggesting kale is laughable. Also, the risk calculators oversimplify complex genetics and lifestyle interactions. Bottom line: don’t trust every line of advice, do your own digging.
Michael Coakley
November 10, 2025 AT 09:20Ah, the age‑old quest for eternal rigidity – a noble pursuit, if you enjoy feeling like a statue at a museum. Philosophically speaking, bones are the ancient archives of our lived moments, mineralized stories etched in calcium. Yet we treat them like disposable housing, neglecting the silent erosion that time and habits bring. So perhaps the secret lies not in more supplements, but in mindful movement that honors the marrow’s whisper. Or maybe just stop overthinking and jog a bit – the universe loves irony.
Leslie Woods
November 23, 2025 AT 02:54Bone health matters, period.
Manish Singh
December 5, 2025 AT 20:27I hear you all – staying active and getting enough vitamin D can be tough, especially when life gets busy. I’ve seen friends improve their bone density just by taking short walks after meals and swapping soda for fortified orange juice. It’s the little, consistent steps that add up, and your body will thank you with stronger bones over time.
Dipak Pawar
December 18, 2025 AT 14:00When we interrogate the osteogenic cascade, the interplay of mechanotransduction and endocrine signaling emerges as a pivotal axis for skeletal resilience. The primary conduit for this dialogue is the Wnt/β‑catenin pathway, which orchestrates osteoblast differentiation in response to micro‑strain stimuli. Empirical data from longitudinal cohort studies indicate that weight‑bearing activities amplify cortical thickness by up to 12% over a decade, contingent upon adequate serum 25‑hydroxyvitamin D levels. Moreover, dietary calcium bioavailability is modulated by gut microbiota composition, with Lactobacillus strains facilitating enhanced absorption via acidic pH microenvironments. In populations with prevalent lactose intolerance, fortified plant‑based milks provide comparable bioavailable calcium, though the matrix effect of phytates must be mitigated through food preparation techniques such as soaking and fermentation. Concurrently, the catabolic influence of chronic glucocorticoid exposure can be attenuated by intermittent high‑intensity interval training, which stimulates osteocyte apoptosis reversal mechanisms. It is also critical to recognize the hormonal interdependence of estrogen and testosterone in preserving trabecular architecture; post‑menopausal women benefit markedly from selective estrogen receptor modulators combined with resistance training protocols. Nutraceuticals such as kelp‑derived iodine and magnesium citrate further support hydroxyapatite crystallization, enhancing mineral density. Thus, a multifactorial regimen encompassing biomechanical loading, optimized micronutrient intake, gut microbiome stewardship, and endocrine modulation constitutes the most robust strategy for mitigating age‑related osteopenia.
Naomi Ho
December 31, 2025 AT 07:34Great breakdown, Dipak.
Just a quick add – don’t forget the simple step of getting sunlight for vitamin D, especially in winter months. Even 10‑15 minutes a day can make a big difference without the need for pricey supplements. Also, regular check‑ups with a DEXA scan can track progress and catch issues early.
Jonathan Alvarenga
January 13, 2026 AT 01:07Here’s the thing: you can pile on every piece of advice in the world, yet the underlying systemic issue remains untouched. The healthcare model treats bone health as an afterthought, relegating it to the sidelines of primary care. So you get this endless list of supplements, exercise regimens, and dietary tweaks that sound solid on paper but lack real accessibility. For low‑income communities, a daily calcium tablet is a luxury, let alone a gym membership for weight‑bearing workouts. Then there’s the pharmaceutical push for bisphosphonates, which come with their own suite of side effects, creating a dependence loop that doesn’t solve the root cause. We need policy‑level interventions: food fortification programs, community‑based exercise initiatives, and affordable screening. Until those structural changes happen, these “tips” are just a veneer over a deeper neglect of bone health in public health planning. So while you’re busy counting servings of kale, the real battle is for equitable access to bone‑protective resources.
James McCracken
January 25, 2026 AT 18:40Interesting points, Jonathan, but let’s not throw the baby out with the bathwater. While systemic reforms are essential, dismissing individual agency can be counterproductive. Personal lifestyle choices still wield substantial influence over bone density, especially when combined with emerging research on the gut‑bone axis. It’s a delicate balance between macro‑policy and micro‑behavior; both are necessary for a truly comprehensive approach.
Jim McDermott
February 7, 2026 AT 12:14Hey all, just wanted to say I’ve started swapping soda for kefir and taking a short walk after dinner. I’ve noticed less joint stiffness and feel more energetic, which is a nice bonus.
Christine Watson
February 20, 2026 AT 05:47Keep your chin up, everyone! Small steps add up, and before you know it, you’ll be dancing through life with stronger bones and a brighter smile.